Case review
Basic information
The patient, a 72 year old female, was hospitalized due to
post activity palpitations and shortness of breath. During the
hospitalization, a large cystic solid mass in the pelvic cavity was
accidentally discovered by abdominal ultrasound. The patient
has no other symptoms except for coughing and expectoration.
Gynecological examination: palpable mass of fetal head size in
pelvic and abdominal cavity, Medium texture, no tenderness,
moderate in activity.
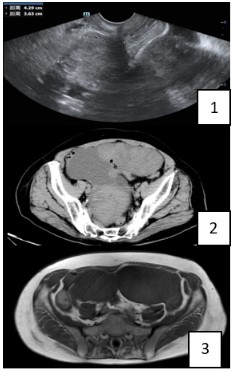
Imaging examination
Ultrasonography shows a 14.2 x 6.9 cm cystic solid mixed
light mass with clear boundary can be seen in the pelvic cavity,
mainly cystic, considering the possibility of Cystadenoma (Figure 1). CT shows that multiple round like solid masses are seen
in the lower abdomen and pelvis, and some of them are cystic,
with uneven internal density and clear boundary. The source of
accessories should be considered as neoplasm (Figure 2). MRI:
Multiple lumps of equal or slightly longer T1 or slightly longer T2 mixed signal shadows can be seen in the lower abdomen
pelvic cavity, with irregular morphology, and the larger ones are
about 11.3 cm in size × 7.9 cm × 10.6 m, the boundary is not
clear, the solid part of the enhanced scan is slightly uneven enhanced, showing delayed enhancement, and the cystic component is not significantly enhanced, considering neoplasm: may
be sex cord-stromal tumours or cystadenoma (Figure 3).
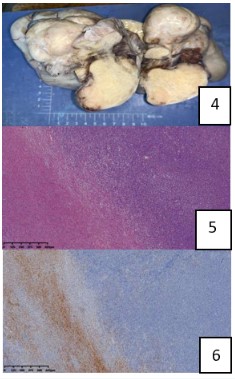
Gross morphology
There is a huge cystic solid mass in the pelvic cavity, approximately 21.5 cm x 19 cm x 10 cm, with a smooth surface and a
lobulated shape. The solid part has a tough gray white material
on the cut surface, and the cystic area contains a light yellow
clear liquid.
Pathological diagnosis
Microscopically, most of the areas are spindle shaped cells
with mild atypia, accompanied by edema and hyaline degeneration; In local areas, a large number of atypical small round cells
can be seen diffuse infiltration; The cystic area contains a light
yellow clear liquid, and the cyst wall is covered with a single
layer of flat epithelium.
Diagnosed as that the spindle cell region is ovarian theca fibroma, the cystic region is serous cystadenoma, and the small
round cell region is non Hodgkin’s diffuse large B-cell lymphoma
(non germinal center origin).
Note: Considering that the majority of this tumor is follicular
fibroadenoma and the lymphoma is only a focal lesion, it is considered to be an invasion of lymphoma in other parts. Please
further clarify the source of lymphoma in combination with
other examinations in clinical practice.
Discussion
Clinical characteristics
Follicular fibroadenoma usually occurs in perimenopausal
or postmenopausal women, with an average age of around 60
years [3]. Common symptoms include postmenopausal bleeding or irregular menstruation, as well as non-specific symptoms
such as abdominal pain or enlargement caused by tumor compression or bleeding. In a few cases, ascites may be present,
and the occurrence of acute abdomen may indicate the occurrence of pedicle torsion of the tumor; Clinical symptoms may be
related to estrogen levels. There are also literature reports of
follicular fibroadenoma that occurs during pregnancy, and this
tumor can also be associated with other gynecological diseases
(such as uterine leiomyoma, endometriosis, teratoma, polycystic ovary syndrome, etc.) [4].
Imaging manifestations
Follicular fibroadenoma often presents as a circular or quasi
circular mass on imaging, mostly occurring on one side with
clear boundaries and complete capsule. Larger tumors may
manifest as compression on surrounding tissues; Enhanced
signals can manifest as uneven enhancement, with gradual delayed enhancement [5,6].
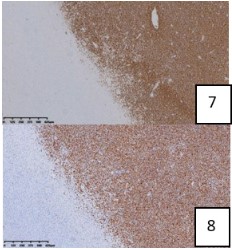
Pathological features
Generally, it appears as gray white nodules, with most nodules being solid, some may be accompanied by cystic changes,
and a few may be accompanied by calcification and bleeding
[4]. Microscopically, the tumor is composed of milder spindle
shaped cells with mild cell atypia, arranged in a flowing or
patchy pattern, and may be accompanied by interstitial edema,
hyaline degeneration, and calcification; Vimentin and sex cord
stromal cell markers inhibin, Calletinin, and SF-1 were all positively expressed in tumors [1].
Conclusion
In summary, the dual primary tumor of follicular fibroadenoma combined with lymphoma in this case is extremely rare.
Based on its clinical and pathological characteristics, this article carefully identifies the underlying lymphoma components.
Looking back at this case, the lymphoma component is focal,
and it is necessary to remind the pathologist that when the tumor component is complex and uneven in texture, extensive
and sufficient sampling should be taken to avoid missed diagnosis. At present, there is no unified standard for the treatment
of dual primary tumors, and the treatment plan needs to be
determined individually [7]. However, determining an individualized treatment plan depends on clinical multidisciplinary discussions. Clinicians should strengthen their understanding of
the disease, identify the primary site of lymphoma based on
clinical data, and proceed with the next step of treatment under
the guidance of multiple disciplines.
References
- WHO Classification of Tumours Editorial Board ed. World Health
Organization classification of tumours. 5th ed. Female genital
tumours. Lyon: IARC Press. 2020.
- Cree IA, White VA, Indave BI, Lokuhetty D. Revising the WHO
classification: Female genital tract tumours. Histopathology
2020; 76: 151-156.
- Kurman RJ, Carcangiu ML, Herrington CS, Young RH. eds. World
Health Organization classification of tumours of female reproductive organs. Lyon: IARC Press. 2014.
- Alerman A. Ovarian pathology. Curr Opin Obstet Gynecol. 1992;
4: 608-615.
- Paladini D, Testa A, Van Holsbeke C, Mancari R, Timmerman D, et
al. Imaging in gynecological disease (5): Clinical and ultrasound
characteristics in fibroma and fibrothecoma of the ovary. Ultrasound Obstet Gynecol. 2009; 34: 188-195.
- Sivanesaratnam V, Dutta R, Jayalakshmi P. Ovarian fibroma-clinical and histopathological characteristics. Int J Gynaecol Obstet.
1990; 33: 243-247.
- Vogt A, Schmid S, Heinimann K, et al. Multiple primary tumours:
challenges and approaches, a review. ESMO Open. 2017; 2:
e000172.