Introduction
Subungual eccrine poroma is one of the rare benign tumors
originated from sweat glands, the gold standard for diagnosis
of which is histopathology. Due to the particularity of the subliungual eccrine poroma, the rash of subungual eccrine poroma
has no obvious specificity and no obvious symptoms, and it is
easy to delay treatment and misdiagnosis. The use of dermoscopy and reflective confocal microscopy has improved the diagnosis of subungual tumors including eccrine poroma. Here we
reported a case of subungual eccrine poroma which provided
direction for its diagnosis and surgical resection by dermoscopy
and reflectance confocal microscopy as auxiliary tools.
Case presentation
A 71-year-old woman, a housewife, visited our outpatient
complained with the mass under the nail on the right middle
finger over 40 years. It began as a invasive erythema with clear border under the lateral margin of the middle finger nail, without pain or itching. The erythema slowly enlarged with the
rough and thickened surface, occasionally rupturing or bleeding. The patient did not report previous trauma or surgeries.
There was no positive family history.
General examination did not reveal any abnormalities. Dermatological examination showed a invasive red plaque, with
rough surface, erosion scab under the lateral edge of the middle
finger nail, with the size of 0.5 cm × 1.5 cm and the brown spots
on the nail surface (Figure 1), without tenderness. Examination
of the axilla did not reveal lymphadenopathy.
Laboratory results showed normal blood cell counts, blood
chemistry and coagulation function. Dermoscopy revealed the
pink background, morphological vascular structure, atypical
hairpin vessels, focal spherical or circular coiled vessels, scattered pink ball, white halo, yellow white, pink without structural area, and purple brown bleeding spots under the nail bed were
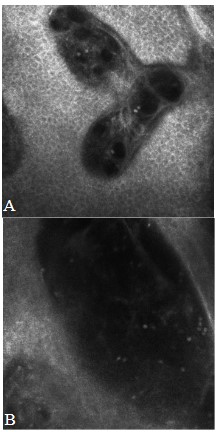
observed (Figure 2). RCM showed mild hypertrophy of the epidermis, tumor mass in the dermis, with more cystic and lumen-like structures and a low refractive profile and heterogeneous
cell structure. Superficial dermis vessels were significantly dilated and congested, and there was little infiltration of inflammatory cells around the canal (XZ scan) (Figures 4A,4B), which
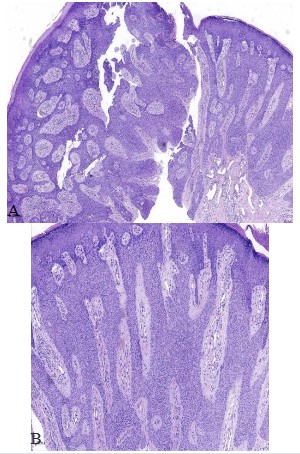
suggested eccrine poroma. Skin biopsy was performed and the
histopathology showed that the mild hypertrophic epidermis,
visible tumor mass connected to the epidermis composed of
small basal cells with a downgrowth pattern, without peripheral
palisaded arranged cells. The dermal vessels were significantly
dilated, with a few of inflammatory cells infiltration (Figures
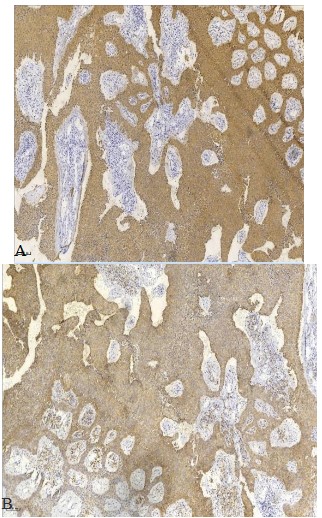
5A,5B). Immunohistochemistry showed the positve results for
EMA and CK, scattered positivefor Bcl-2 and negative for CEA
and S100. About 10 percent cells of the tumor was postive for
Ki67 (Figure 6). The final diagnosis was made as subungual eccrine poroma.
The patient underwent a tumor resection under the local anesthesia. Dermoscopy after nail extraction showed invasive erythema and dilated capillaries involved almost all of the nail bed
surface, the yellow-white interlaced area around the vessels,
and pink balls (Figure 3). During the operation, the tumor was
surgically removed completely directed by the dermoscope.
There was no recurrence by follow-up for half a year.
Dermoscopy after nail extraction showed invasive erythema
and dilated capillaries involved almost all of the nail bed surface, the yellow-white interlaced area around the vessels, and
pink balls (× 50).
Mild hypertrophy of the epidermis, tumor mass in the dermis, with more cystic and lumen-like structures and a low re-
fractive profile and heterogeneous cell structure (4A). Superficial dermis vessels were significantly dilated and congested,
and there was little infiltration of inflammatory cells around the
canal (4B) (XZ scan).
The mild hypertrophic epidermis, visible tumor mass connected to the epidermis composed of small basal cells with a
downgrowth pattern, without peripheral palisaded arranged
cells. The dermal vessels were significantly dilated, with a few of
inflammatory cells infiltration (5A HE staining ×50; 5B HE staining ×100).
The immunohistochemistry showed the positve results for
EMA (6A) and CK (6B) (SP staining ×100).
Discussion
Eccrine poroma is one of the benign cutaneous appendage tumors differentiated into the terminal sweat gland duct
which originates from the eccrine gland duct component in the
dermis and epidermis. Generally, it is commonly found in the
palmoplantar area with rich eccrine glands, such as the lateral
edge of the palmoplantar of the foot. Ocassionally it is also reported to occur in the trunk, eyelid, subungual sites and so on
[2,3]. Eccrine poroma is relatively rare and only about 10% of
the sweat gland tumors, which account for 1% of primary skin
tumors [1]. Most patients are over 40 years of age [4]. Typical
clinical manifestations are solitary, soft skin color to red papules
or nodules and subungual eccrine poroma is rarely reported,
only with more than 10 cases reported by pubMed search. The
etiology and pathogenesis of eccrine poroma are unclear, which
are related to solar injury, radiation exposure, trauma and human papillomavirus infection.
The diagnosis of subungual eccrine poroma is mainly based
on the histopathological examination [4]. Its typical histopathological findings include the the well-demarcated tumor located in the upper part of the epidermis extending from the
epidermis to dermis with clear demarcation between normal
keratinocytes with the tumor cells, and dilated dermal capillaries rounded with little lymphocytes. Tumor cells are cubical or
round basal cells with the uniform size round and deep nucleus,
some with transparent cytoplasm, with tight intercellular junctions and peripheral palisaded arrangedment. Clinically, it is difficult to take the biopsy for the subungual eccrine poroma for
the special anatomical location.
Recently dermoscopy and RCM have been favored clinically
for their non-invasive, painless and fast features. Therefore,
they are of great significance in the diagnosis of nail-related
diseases and provide a reference for the preliminary diagnosis
of diseases. The main manifestations of eccrine poroma under
dermatoscopy are multiple red space, glomerular vessels, hairpin vessels with floral and foliar vascular and polymorphism
vascular pattern, spherical/lacunar structure, frog egg appearance and acne opening [5], which can provide important
clues for the diagnosis of subungual eccrine poroma. The RCM
features of subungual eccrine poroma include multiple cystic
cavity, lumen-like structure and a low refractive profile. The
polymorphic vascular structures and scattered pink globules
correspond to the tortuous and dilated capillaries in the nail
bed and the rich capillary structures in the interstitium. Pink-white unstructured areas and white to pink halos were associated with specific histopathological features, including fibrotic
tissue proliferation and fibrinoid oedema surrounding several
dilating vessels, respectively [6]. Among the RCM parameters,
"fence-less cord", "dark hole," "prominent vascularization" and
"rich matrix" were positively associated with eccrine poroma
in the univariate analysis. By the cluster analysis, RCM features
correspond to 97% with the histopathological diagnosis of eccrine poroma in cases [7]. In our case, a tumor mass was visible
in the dermis of RCM, with more cystic cavity and luminal structures and without heteromorphous cells, which conformed to
the RCM characteristics of eccrine hidradenoma.
With skin imaging techniques, subungual eccrine poroma
should be differentiated from other nail diseases such as ony-chomycosis, nail psoriasis, subungual squamous cell carcinoma,
subungual hemorrhage and subungual malignant melanoma,
and so on, all of which can cause nail changes such as nail loss
or nail dissection. But each of them has corresponding typical clinical manifestations. Onychomycosis involving the nail desk
showed the tip of the serrated scales is facing the proximal end
and the high refractive structure was observed under the deck
with RCM. In nail psoriasis, yellow and white flocculent can be
seen above and below the diseased nail, untypical vascular dilation on the reddish base of nail bed, white, unstructured area,
yellow and white scales. Hyperplastic, dilated capillaries in the
dermal papilla and inflammatory cells infiltration can be seen
by RCM. Subungual Squamous Cell Carcinoma (SSCC) is characterized by black or red lines, irregular blood vessels, and patchy
bleeding or diffuse homogeneous stain in the subungual haemorrhage by dermoscopy. Under the RCM, SSCC was discovered
the disorganized skin structure with focal distribution of nucleated cells in the epidermis and dermis, abnormal keratinocytes
in the prickle layer and typical hornbead structure. Dark areas
were observed under the deck with RCM, and no obvious pigment particles were observed. Subungual melanoma melanoma shows an irregular brown pigmented band of different
shades and widths with a width greater than 3mm with positive
Hutchinson sign. With RCM, subungual in-situ malignant melanoma is characterized by single proliferation of melanocytes.
Melanocytes are distributed irregularly in the basal layer with
atypia and concentrated chromatin. Subungual invasive malignant melanoma often involves the subdermis, with obvious cell
atypia and invasive growth pattern.
In our case, dermoscopy and RCM showed the typical imaging findings of subungual eccrine poroma, which was very
helpful for clinical diagnosis. Morerover, the invasive scope of
the tumor was fully exposed under the dermoscopy during the
surgical treatment, which provided a reference scope of surgical resection to completely remove the tumor. Dermoscopy and
RCM, as a new auxiliary examination and diagnosis techniques
are helpful for the diagnosis and treatment by operation of subungual eccrine poroma.
Funding sources
Chongqing Science and Health Joint Medical Research Project: Clinical Application of Partial Removal of Nail Bed and Nail
Matrix Combined with Skin Imaging Technology in the Treatment of Melanocytic Diseases (2021 MSXM118).
References
This study shows that when epidural bupivacaine-fentanyl is administered either through intermittent or continuous method, it provides stable and comparable haemodynamic effects, sensory block height and comparable incidence of side effects for major gynaecological surgeries. We recommend that continuous and intermittent epidural anaesthesia with bupivacaine-fentanyl should be used for major gynaecological surgeries, with a preference for intermittent method as it provides more stable haemodynamic effects with lesser volume of local anaesthetic agent with fentanyl.
References
- Li J, Ding Y, Zhang S, He W. Eccrine poroma: A case report. Asian
J Surg. 2023; 46: 874-875.
- Yorulmaz A, Aksoy GG, Ozhamam EU. A Growing Mass under the
Nail: Subungual Eccrine Poroma. Skin Appendage Disord. 2020;
6: 254-257.
- Mencía-Gutiérrez E, Navarro-Perea C, Gutiérrez-Díaz E, Cámara-Jurado M, Bengoa-González Á. Eyelid Eccrine Poroma: A Case
Report and Review of Literature [J]. Cureus. 2020; 12: e8906.
- Chessa MA, Patrizi A, Baraldi C, Fanti PA, Barisani A, et al. Dermoscopic-Histopathological Correlation of Eccrine Poroma: An
Observational Study. Dermatol Pract Concept. 2019; 9: 283-291.
- Göktay F, Güneş P, Akpolat ND, Ferhatoğlu ZA, Önenerk M. Periungual Eccrine Poroma Masquerading as Ingrown Toenails. A
Case Report with Dermoscopic Findings. J Am Podiatr Med Assoc. 2017; 107: 551-555.
- Takada T. Diagnostic features of a non-pigmented eccrine poroma with a collarette: Histopathological and dermoscopic correlation. Clin Case Rep. 2021; 9: 1601-1604.
- Di Tullio F, Mandel VD, Ignazio S, Cinotti E, Kaleci S, et al. The
role of reflectance confocal microscopy in the diagnosis of eccrine poroma: A retrospective case-control study. Exp Dermatol.
2022; 31: 1779-1790.