Introduction
Violence is a substantial cause of morbidity and mortality among women around the world. According to the World
Health Organization, 1 in 3 women experience physical and/or
sexual violence in their lifetime [1]. Among bisexual and non-monosexual (have partners of multiple sexes/genders) women,
the percentage of gender-based violence rises to 61% and 78%
respectively [2]. This violence places an immense burden on individuals, healthcare systems, and societies around the world.
In the United States, the economic toll due to violence
against women is estimated to be over $8.3 billion dollars yearly
[3]. An estimated $4.2 billion is spent annually on the costs of
physical assault alone [3]. Prevention strategies aimed at reducing cases of violence against women can have immense downstream cost saving benefits.
Violence is associated with an increased relative risk of both
overall and diagnosis-specific hospitalizations among women
[4]. Most victims historically suffer repeated violence, and up to
one third of these cases involve a weapon, such as a knife, club,
or gun [5]. Due to safe disposition challenges and the severity of injuries, treatment often involves lengthy hospital stays
and the development of chronic conditions [4,6]. Women are
most likely to experience interpersonal violence by a familiar
perpetrator, commonly a husband or close family member with
whom they share living space [4]. This can make it challenging
to discharge from the hospital to a safe environment. Women
with past exposure to interpersonal violence are more likely to
be admitted to the hospital with re-injury, somatic symptoms,
and mental health sequelae [6]. These mental health sequelae include clinical depression, post-traumatic stress disorder
(PTSD), and substance use disorder [4].
Examining the impact of violence against women is challenged by historical underreporting [7,8]. Many of these cases
go unreported due to fear of personal and societal consequences, economic codependence, and emotional strain [8]. Furthermore, medical research examining violence towards women
has been challenged by underfunding. A study on the allocation of National Institute of Health funds found that funding for
interpersonal violence decreased by $95 million from 2008 to
2019 [27]. In contrast, funding for Alzheimer’s disease and dementia increased by $1.8 billion dollars [27].
Trends, risk-factors, and outcomes of violence against women have not been well studied at the U.S. national level. Using the National Trauma Data Bank, the present study exam-
ines data from 2007-2019 in the United States. This database
study aims to identify risk factors and outcomes of violent injury
towards women to better inform public health prevention, resource optimization, and clinical management efforts. We hypothesize that there exist significant differences in violent injury
towards women on the basis of demographic variables such as
insurance status, substance usage and race.
Methods
Research design and IRB approval
This is a retrospective cohort study of hospitalized injured
patients in the United States National Trauma Data Bank (NTDB)
from 2007-2019. The National Trauma Data Bank is a nationally
sourced trauma registry owned and operated by the American
College of Surgeons. It includes entries from public and private
hospitals across the country. The data bank includes patients
with traumatic injuries admitted to trauma centers based on
a patient inclusion criteria algorithm [9]. This dataset included
records from 1,153 unique hospitals, 628 of which are ACS verified at Level I, II, III, or IV. The overall participation rate of trauma centers in 2019 is 46.19%. Participant use file request for
the study’s objectives was approved by the American College of
Surgeons Trauma Quality Program and data was obtained from their online Participant Use Files (PUF) [10]. Additionally, IRB approval was obtained through the University of Vermont (Committee on Human Research in the Medical Sciences ID: 17-0467).
Inclusion and exclusion
We included all female patients aged 13 years and over who
had injuries as a result of violence, as identified by International
Classification of Disease (ICD) external cause codes in the NTDB
from 2007-2019. Patients with ICD-9 or ICD-10 external cause
codes with intent of “assault” were considered victims of violence. Patients with ICD external cause codes of “unintentional”
or “self-inflicted” were considered to be injured non-violently;
cause codes “other” and “undetermined” were excluded.
Data collection and variables
Data were obtained from the Trauma Quality Improvement
Program (TQIP) National Trauma Data Bank Participant Use Files
(NTDB PUFs) from 2007 to 2019. PUFs for all data years were
combined for analysis. Data elements available included patient demographics, information on injury severity (abbreviated
injury severity score), vital signs, payer information, transport
mode, and pre-hospital care. ICD-9 and ICD-10 procedure, diagnosis, mechanism, and external cause codes were used. Comorbidities included coronary artery disease, bleeding disorders
and anticoagulation, cirrhosis, chronic obstructive pulmonary
disease, cerebrovascular accidents, dementia, diabetes, cancer,
congestive heart failure, hypertension, peripheral arterial disease, psychiatric or personality disorders, smoking, substance
abuse, alcoholism and others collected in the TQIP NTDB database. Toxicology positive screening results were used to identify
drug and alcohol intoxications.
Outcome variables included hospital length of stay, discharge disposition, mortality, and hospital complications. Hospital complications evaluated were wide-ranging, and included
bleeding, coagulopathy, infection (sepsis, deep and superficial
surgical site, central line, osteomyelitis, pneumonia and urinary
tract infections), myocardial infarction, cerebrovascular accident, kidney injury, venous thromboembolism, compartment
syndrome, return to OR, unplanned ICU, and others collected in
the TQIP NTDB database.
Facility keys were also obtained from TQIP, which allowed
for grouping of patients into the hospital at which they were
treated. Independent variables included violent injury, mortality, and hospital length of stay. The MGAP scale (Mechanism,
GCS, Age, and Penetrating injury) was also used to control
for mortality probability, as it has been found to significantly
outperform other injury classification scores [25]. Dependent
variables included incident information, mechanism of injury,
patient demography, injury patterns and severity, physiologic
derangement, and available hospital resources. Missing variables were evaluated for both groups.
Statistical analysis
Patient characteristics, injury patterns, physiology, care utilization, complications and in-hospital trauma mortality data
were analyzed. Univariate statistics, including counts, percentages, means with SDs, medians with IQRs, t-tests, Wilcoxon
rank-sum tests, and Pearson χ2 tests, were used to compare patient and injury characteristics for women with violent and non-violent injuries. Unless otherwise specified, proportions were
calculated using the denominator of all injured women included
in the sample, and reflect only the patterns of injury presenting
to U.S. Trauma Centers, not the true incidence rate in the population. Confidence intervals for proportions were calculated using a logit transform. The Cochran-Armitage test was used to
assess trends (non-stationarity) in violent injury and mortality
patterns over time.
Multivariable logistic regression with stepwise backwards
elimination (Pr = 0.1) was utilized to identify independent risk
factors for severe injury (ISS > 14), prolonged hospitalization
(length of stay greater than 14 days) and mortality. Variables
considered for stepwise selection in logistic regression models
included age, sex, physiology, race, positive drug and alcohol
toxicology screening, smoking history, health status (as measured by Charlson Comorbidity Index), insurance status, hospital type, and injury severity (ISS). When used as predictors, ISS,
GCS, MGAP, and Systolic Blood Pressure (SBP) were all entered
into the model as continuous variables. Robust standard errors
were calculated for all models, clustering patients at the facility
level. Given that in very large datasets such as NTDB arbitrary
correlations will appear highly “statistically significant” due to
random chance, a p of 0.01 along with an appropriate confidence interval and clinically relevant effect size was used to indicate significance in multivariate models [24].
All statistical analyses were performed using Stata V.17
(StataCorp. 2019. Stata Statistical Software: Release 17. College
Station, Texas: StataCorp).
Results
Patient flow and characteristics
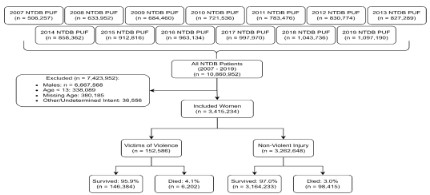
Of the 10.86 million patients in NTDB from 2007-2019, 4.17
million were female, and 3.42 million met inclusion criteria.
In total, 152,586 women (4.3%) were victims of violent injury.
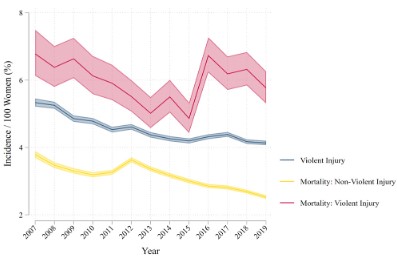
From 2007 to 2019, the proportion of women presenting to the
hospital with violent injury decreased from 5.3% to 4.1%, with
a spike in death rate in 2016 (Figure 2). Case fatality rate for
violent injury was higher than non-violent injury (4.2% vs 3.0%,
p < 0.001). Case fatality rates for both groups decreased significantly over time (Figure 2).
Trends in violent injury
Violent injury mortality, violent injury, and non-violent injury
mortality declined over time, and this trend was found to be statistically significant using the Cochran-Armitage test (p < 0.001
for all). Violent injury incidence and non-violent injury mortality
steadily decreased between 2007 and 2019. Though in-hospital
violent injury mortality increased sharply between 2015 and
2016, by 2019 it returned to pre-2007 levels (Figure 2).
Univariate analysis
Table 1: Patient characteristics by exposure to violence.
|
Exposure to violence |
|
None (n = 3,262,648) |
Victim of Violence (n = 152,586) |
Total (n = 3,415,234) |
| Age (years) [mean, (SD)] |
57.8 |
(22.7) |
35.1 |
(14.6) |
56.7 |
(22.9) |
| Race [%, n] |
| Non-White |
20.9% |
679,801 |
58.1% |
88,230 |
22.6% |
768,031 |
| White |
79.1% |
2,570,045 |
41.9% |
63,750 |
77.4% |
2,633,795 |
| Payment Method [%, n] |
| Medicaid |
10.1% |
309,200 |
36.7% |
51,724 |
11.3% |
360,924 |
| Not Billed (for any reason) |
0.3% |
9,976 |
0.9% |
1,286 |
0.4% |
11,262 |
| Self-Pay |
7.9% |
241,564 |
25.2% |
35,537 |
8.7% |
277,101 |
| Private/Commercial Insurance |
35.2% |
1,079,099 |
21.4% |
30,206 |
34.6% |
1,109,305 |
| Medicare |
41.7% |
1,276,648 |
8.0% |
11,249 |
40.2% |
1,287,897 |
| Other Government |
1.4% |
44,038 |
3.6% |
5,096 |
1.5% |
49,134 |
| Other |
3.3% |
101,833 |
4.1% |
5,755 |
3.4% |
107,588 |
| Length of Stay (days) [mean, (SD)] |
5.3 |
(6.8) |
4.3 |
(7.4) |
5.2 |
(6.8) |
| Total GCS [mean, (SD)] |
14.3 |
(2.3) |
14.0 |
(2.9) |
14.3 |
(2.4) |
| Hospital Complications [%, n] |
| None |
86.3% |
2,814,187 |
88.1% |
134,472 |
86.3% |
2,948,659 |
| Complications |
13.7% |
448,461 |
11.9% |
18,114 |
13.7% |
466,575 |
| Mortality [%, n] |
| Lived |
97.0% |
3,164,233 |
95.9% |
146,384 |
96.9% |
3,310,617 |
| Died |
3.0% |
98,415 |
4.1% |
6,202 |
3.1% |
104,617 |
Risk factors
Populations with highest odds of violent injury included
Black, Native American, Hispanic or Latina, uninsured, and Medicaid insured women. Black race was the highest independent
predictor of violent injury (OR 2.88, 95% CI 2.63; 3.15, p<0.001),
followed by Native American women (OR 2.50, 95% CI 2.06;
3.03, p<0.001). Older patients were less likely to present with
violent injury than their younger counterparts (10-year OR 0.78,
95% CI 0.77; 0.79, p<0.001) (Table 2, Model 1). Positive drug
and alcohol screening were also found to be independently associated with violent injury, including cocaine, alcohol, and/or
amphetamines, as well as patient history of smoking and/or
substance use disorder (Table 2, Model 1).
Violent injury was found to be associated with a 36.5% higher odds of in-hospital mortality when controlling for other risk
factors (OR 1.37, 95% CI 1.21; 1.54, p<0.001) (Table 2, Model 2).
Patients with greater injury severity (lower GCS, lower SBP, higher ISS) had higher odds of in-hospital mortality (Table 2, Model
2), and prolonged (>14 days) hospital stay (Table 2, Model 3).
Patients with lower injury severity as measured by MGAP had
lower odds of in-hospital mortality, and higher estimated odds
of prolonged hospitalization. When controlling for other risk
factors, uninsured status was associated with greater odds of
in-hospital mortality (OR 1.71, 95% CI 1.57; 1.87, p<0.001) (Table 2, Model 2). Other risk factors for prolonged hospital stay included increased age, history of alcoholism, history of psychiatric or personality disorders, and severe injury (Table 2, Model 3).
Positive alcohol screening and smoking history were associated
with lower odds of prolonged hospital stay (Table 2, Model 3).
Multivariate analysis
Table 2: Logistic regression models predicting violent injury and mortality among women,
and hospitalization among violently injured women
|
(1) Violent Injury |
(2) Mortality |
(3) Prolonged Hospitalization |
| Age (10-year) |
0.778*** |
1.584*** |
1.193*** |
|
[0.768,0.789] |
[1.549,1.620] |
[1.148,1.240] |
| Ethnicity: Hispanic |
1.374*** |
1.001 |
0.868 |
|
[1.269,1.488] |
[0.898,1.116] |
[0.724,1.040] |
| Race: Native American |
2.500*** |
0.832 |
0.804 |
|
[2.060,3.034] |
[0.626,1.106] |
[0.539,1.200] |
| Race: Asian |
0.979 |
1.088 |
0.979 |
|
[0.847,1.132] |
[0.937,1.265] |
[0.613,1.565] |
| Race: Black |
2.875*** |
1.139 |
1.105 |
|
[2.627,3.146] |
[0.993,1.306] |
[0.885,1.381] |
| Race: White |
0.764*** |
1.090 |
0.941 |
|
[0.701,0.833] |
[0.974,1.220] |
[0.768,1.151] |
| (+) Alcohol Screening |
1.447*** |
0.755*** |
0.666*** |
|
[1.385,1.511] |
[0.689,0.828] |
[0.592,0.750] |
| (+) Drug Screening |
1.231*** |
0.840*** |
1.248*** |
|
[1.184,1.281] |
[0.790,0.894] |
[1.114,1.398] |
| Insurer: Medicaid
| 2.754*** |
1.115** |
1.116 |
|
[2.550,2.973] |
[1.039,1.197] |
[0.986,1.263] |
| Insurer: Self |
2.424*** |
1.711*** |
0.817* |
|
[2.220,2.645] |
[1.566,1.870] |
[0.694,0.963] |
| Comorbid: Smoking |
1.493*** |
0.712*** |
0.717*** |
|
[1.428,1.562] |
[0.662,0.765] |
[0.636,0.808] |
| Comorbid: Alcoholism |
1.039 |
1.122* |
1.289** |
|
[0.990,1.091] |
[1.015,1.241] |
[1.093,1.520] |
| Comorbid: Psych. Disorder |
1.088*** |
0.892*** |
1.205** |
|
[1.044,1.135] |
[0.838,0.950] |
[1.059,1.372] |
| Comorbid: Substance Abuse |
1.449*** |
0.723*** |
1.154* |
|
[1.381,1.520] |
[0.657,0.796] |
[1.009,1.320] |
| Violent Injury |
— |
1.365*** |
— |
|
|
[1.209,1.542] |
|
| GCS |
— |
0.761*** |
0.864*** |
|
|
[0.749,0.772] |
[0.841,0.887 |
| SBP (mmHg) |
— |
0.993*** |
0.997** |
|
|
[0.992,0.994] |
[0.995,0.999] |
| ISS |
— |
1.084*** |
1.096*** |
|
|
[1.081,1.087] |
[1.088,1.104] |
| MGAP |
— |
0.979** |
1.071*** |
|
|
[0.966,0.993] |
[1.046,1.097] |
| Observations |
481351 |
460036 |
36023 |
| Pseudo R2 |
0.174 |
0.415 |
0.182 |
| AIC |
195970.8 |
78554.8 |
12764.8 |
| BIC |
196137.0 |
78775.5 |
12926.2 |
| Log lik. |
-97970.4 |
-39257.4 |
-6363.4 |
Exponentiated coefficients; 95% confidence intervals in brackets.
Models (1) and (2) are run on the whole sample, and (3) only on patients with violent injury.
Standard errors were clustered at the facility level.
* p < 0.05, ** p < 0.01, *** p < 0.001
Discussion
A better understanding of violence against women can be
achieved by evaluating independent predictors of violence and
outcomes. While there are studies examining the economic and
medical burden of violence against women, there is a lack of
research on independent predictors of outcomes among these
patients [12]. Without detailed analyses and understanding of
independent predictors, it is difficult to develop targeted interventions to reduce mortality rates.
Among a national cohort of hospitalized trauma patients
in the United States, we found a reduction in the proportion
of violent injury among women from 5.2% in 2007 to 4.1% in
2019. This finding is consistent with a recent study examining
the epidemiology of violence against women, which attributes
the decline in violent injury to decreased rates of marriage, increased access to domestic violence resources, and improvements in female economic status [13]. However, in 2016 there
was a marked increase in the death rate for violent injury. This
could be attributable to the changes in the data collecting system transitioning from ICD-9 to ICD-10 [26]. Further investigation must be performed to fully understand this spike in death
rate.
Although violence towards women has been downtrending
over the last several decades, there is an increase in reports of
violence towards women since the start of the COVID-19 pandemic [14]. Social distancing and isolation kept more women
in the home, where they faced increased risk of partner and
family violence [15]. Fear of joblessness and financial hardships also contributed to increased gender-based violence [15].
Prior studies indicate that the loss of income, marriage, and
substance use are risk factors for violence [16]. Future studies
using national databases could evaluate the impact of the pandemic on hospitalizations and outcomes among women due to violence. The present study reports that there was an overall
reduction in the proportion of violent injury towards women
from 2007-2019. Given that the COVID-19 pandemic restrictions have largely been lifted, we predict that the reduction in
violent injury seen prior to COVID-19 may persist. Further research must be conducted in the coming years to fully evaluate
the trends of violence injury against women.
The current study found that independent predictors of higher odds of in-hospital mortality due to violent injury included
smoking, positive cocaine, alcohol, or amphetamine screenings,
and the patient’s history of psychiatric or personality disorders,
or substance use disorder. These findings align with prior studies identifying alcohol and drug use, income status, and mental
health as predictors of interpersonal violence [17]. However,
the correlation between violent injury and risk-adjusted mortality has not been demonstrated at a national scale. Among a national cohort, when controlling for age, physiologic parameters,
and injury severity, we found that there was a 37% increased
odds of in-hospital mortality with violent injury among women
treated at U.S. Trauma Centers.
In our study, regression analysis demonstrated that additional independent predictors of violent injury included identifying as Black, Native American, Hispanic or Latina ethnicity,
uninsured, or Medicaid insured. Among racial demographics,
women in these particular racial groups had the highest odds of
violent injury and in-hospital mortality. This aligns with existing
literature, including one study exploring violence against Native
American and Alaska Native women, which demonstrates that
Native American women have higher rates of physical violence
than Non-Hispanic White women (55.5% vs. 34.5%) [18].
Future work could examine the rates and odds of mortality in cases of violence against gender-queer, non-binary, and
transgender individuals. Current literature primarily explores gender-based violence among bisexual and non-monosexual
women [2]. Efforts to expand the study to include non-binary
gender classifications may lead to more targeted interventions.
Another avenue for further research is examining the incidence
of repeat hospitalizations after violent injuries and prevention
mechanisms currently in place within healthcare settings, as
prevention programs have been successful in decreasing the
rate of violence [19]. It is important to consider that at-risk
women in minority and socioeconomically disadvantaged populations may be underrepresented in the statistics because of
limitations in access to care [8]. This may additionally be confounded by lack of insurance and historical harm by the medical
establishment [8]. Offering targeted support to at-risk women
could encourage seeking medical treatment and longer-term
support as well.
Limitations
There are demographic, generalizability, and data limitations
to this study. A major limitation of this study is that it only evaluates injured patients that present to hospitals and does not
capture violent injuries that result in pre-hospital death or that
do not present to NTDB participating hospitals. Accordingly, our
comparisons are between violently injured women and non-violently injured women, not to the general population; model
estimates of the impacts of violent injury should be interpreted
with this context. Additionally, before 2021 the National Trauma Data Standard did not include non-binary as an option for
sex classification, and so we are not able to identify non-binary
and transgender individuals in our analysis. Prior studies demonstrate increased prevalence of violence against transgender
populations and poorer health outcomes, suggesting a need
for follow-up work with this national dataset to understand
the characteristics and outcomes of non-binary individuals in
NTDB [20]. As mentioned previously, violence against women
historically suffers from underreporting. The present study data
is based on reported cases of violence, however in reality the
death rate could be much higher.
Another limitation of the study is the spike in incidence of
violent injury between 2015-2016 as seen in Figure 2. This finding may be attributed to changes in reporting and data collection that correspond to this time period. Given this anomaly,
further research must be conducted to determine likely causes
of this spike.
This study also does not address potential intersectionality
of women who may have multiple risk factors for experiencing
violence. Women who fall into multiple modifiable and demographic categories may have a different risk profile and may
require distinct targeted prevention strategies. Among college
students, lesbian, gay, bisexual, and transgender individuals
face disproportionate rates of intimate partner violence [21]. A
study examining the intersection of race and immigration status
further demonstrates the importance of approaching violence
against women from an intersectional lens [22]. The pattern of
injury can also be further qualified by demographic and social
categories.
Female survivors of violence are often the subjects of excessive scrutiny and at times blame, particularly when drugs and
alcohol are involved. The researchers acknowledge that the
data available focuses on the victim and offers no information
on perpetrators of violence. The goal of this study is to identify
demographics at higher risk of violence. Interpersonal violence
is a multi-factorial situation that encompasses social determinants of health that pertain to both the victim and the perpetrator. More literature is needed in order to better understand
circumstances beyond those that focus on the victim.
Conclusion
This paper sought to characterize trends, independent predictors and outcomes of violence towards women using United
States national data. Over the past 12 years, NTDB data demonstrates that the proportion of women presenting to trauma centers with injury from abuse or assault among women presenting to hospitals has decreased from 2007-2019. Although the
overall proportion of violence towards women has decreased
over the last decade, violence remains a significant independent predictor of in-hospital mortality among injured hospitalized women. Among women, injury as a result of violence is associated with higher risk-adjusted mortality. This suggests that
future public health initiatives should target high risk populations informed by independent predictors of violence including
demographics, socioeconomics, mental health and substance
use disorders.
Highlights
• Rates of violence against women in the United States has
decreased over the past decade
• Black, Native American, uninsured and Medicaid insured
women had the highest odds of violent injury
• Controlling for other variables, violent injury was associated with higher odds of mortality
References
- World Health Organization, Addressing violence against women.
Fact Sheets; 2021.
- Coston BM. Power and Inequality: Intimate partner violence
against bisexual and non-monosexual women in the United
States. J Interpers Violence. 2021 Jan; 36(1-2): 381-405.
- Max W, Rice DP, Finkelstein E, Bardwell RA, Leadbetter S. The
economic toll of intimate partner violence against women in the
United States. Violence Vict. 2004 Jun; 19(3): 259-72.
- Fochtmann A, Mittlböck M, Binder H, Köttstorfer J, Hajdu S.
Acute Care Surg.Potential prognostic factors predicting secondary amputation in third-degree open lower limb fractures. J.
Trauma. 2014; 76: 1076-1081.
- Kernic MA, Wolf ME, Holt VL. Rates and relative risk of hospital
admission among women in violent intimate partner relationships. Am J Public Health. 2000 Sep; 90(9): 1416-1420.
- Berrios DC, Grady D. Domestic violence: risk factors and outcomes. West J Med. 1991 Aug; 155(2): 133-135.
- Karakurt G, Smith D, Whiting J. Impact of intimate partner violence on women’s mental health. J Fam Violence. 2014 Oct;
29(7): 693-702.
- Gracia E. Unreported cases of domestic violence against women: towards an epidemiology of social silence, tolerance, and
inhibition. J Epidemiol Community Health. 2004 Jul; 58(7): 536-537.
- Chapman A, Monk C. Domestic Violence Awareness. Am J Psychiatry. 2015 Oct; 172(10): 944-945.
- American College of Surgeons. Data dictionary 2021. The committee on trauma. 2021
- Nathens AB, Cryer HG, Fildes J. The American College of Surgeons Trauma Quality Improvement Program. Surg Clin North
Am. 2012 Feb; 92(2): 441-454.
- Hasler RM, Nuesch E, Juni P, Bouamra O, Exadaktylos AK, Leky
F. Systolic blood pressure below 110 mmHg is associated with
increased mortality in penetrating major trauma patients: multicentre cohort study. Resuscitation. 2012 Apr; 83(4): 476-81.
- Elgar G, Smiley A, Latifi R. Major risk factors for mortality in elderly and non-elderly adult patients emergently admitted for
blunt chest wall trauma: hospital length of stay as an independent predictor. Int J Environ Res Public Health. 2022 Jul; 19(14).
- Saltzman LE. Issues related to defining and measuring violence
against women: response to Kilpatrick. J Interpers Violence.
2004 Nov; 19(11): 1235-1243.
- Huecker MR, King KC, Jordan GA, Smock W. Domestic Violence.
StatPearls. 2022 Sep.
- Sahay MR, Dubey S, Sahoo RK, Kanungo S, Sahoo KC, Pati S.
Health-related challenges and coping strategies among women
during pandemics: a systematic review of qualitative studies.
Front Health Serv. 2022 Apr 15; (2): 847753.
- Marques ES, Moraes CL, Hasselmann MH, Deslandes SF,
Reichenheim ME. Violence against women, children, and adolescents during the COVID-19 pandemic: overview, contributing
factors, and mitigating measures. Cad Saude Publica. 2020 Apr;
36(4).
- Nowotny KM, Graves JL. Substance use and intimate partner violence victimization among White, African American and Latina
women. J Interpers Violence. 2013 Aug.
- Rubenstein BL, Lu LZN, MacFarlane M, Stark L. Predictors of interpersonal violence in the household in humanitarian settings:
A systematic review. Trauma Violence Abuse. 2020 Jan; 21(1):
31-44.
- Fedina L, Shyrokonis Y, Backes B, Schulz K, Ashwell L, Hafner S et
al. Intimate partner violence, economic insecurity, and health
outcomes among American Indian and Alaska Native Men and
Women: Findings from a national sample. Violence Against
Women. 2022 Sep.
- Ellsberg M, Arango DJ, Morton M, Gennari F, Kiplesund S, Contreras M, et al. Prevention of violence against women and girls:
what does the evidence say? Lancet. 2015 Apr; 385(9977):
1555-66.
- Devries K, Knight L, Petzold M, et al. Who perpetrates violence
against children? A systematic analysis of age-specific and sex-specific data. BMJ Paediatr Open. 2018; 2(1).
- Whitfield DL, Coulter RWS, Langenderfer-Magruder L, Jacobson
D. Experiences of intimate partner violence among lesbian, gay,
bisexual, and transgender college students: The intersection of
gender, race, and sexual orientation. J Interpers Violence. 2021
Jun; 36(11-12): NP6040-NP6064.
- Ghafoori B, Matos M, Goncalves M. Dropout from evidence-based trauma treatment in a community mental health clinic
serving victims of interpersonal violence. J Trauma Stress. 2022
Jun; 35(3): 1025-1041.
- Gomez-de-Mariscal E, Guerrero V, Sneider A, et al. Use of the
p-values as a size-dependent function to address practical differences when analyzing large datasets. Scientific Reports. 2021
Oct; 11(20942).
- Mohammed Z, Saleh Y, AbdelSalam EM, et al. Evaluation of the
revised trauma score , MGAP, and GAP scoring systems in predicting mortality of adult trauma patients in a low-resource setting. BMC Emerg Med. 2022 May; 22(1): 90.
- Centers for Disease Control and Prevention. International Classification of Diseases, (ICD-10-CM/PCS) Transition-Background.
https://www.cdc.gov/nchs/icd/icd10cm_pcs_background.htm.
Accessed March 1, 2023.
- Ballreich JM, Gross CP, Powe NR, Anderson GF. Allocation of national institutes of health funding by disease category in 2008
and 2019. JAMA Netw Open. Jan 2021; 4(1): e2034890.