Introduction
Empty sella is usually referred to as a syndrome. It was first
reported by Busch in 1951 as an anatomical condition presenting as the herniation of subarachnoid space into the sella turcica, accompanying flattening of the pituitary gland to the sellar
floor with or without enlargement of the sella turcica. Usually,
it is divided as primary or secondary [1,2]. Here, we report a
case of primary empty sella syndrome with postoperative visual
impairment.
Case report
A 55-year-old female presented with 10 years of recurrent
headache and 3 months of exacerbation. She had no history
of previous illness, and she was married with one son and one
daughter. She had normal menses. On admission, she was in
good general condition and normal on ophthalmologic examination. In addition, the cardiac ultrasound, abdominal ultrasound,
chest CT and ECG were all normal on admission. Laboratory
indices, including blood indices, biochemical indices, electrolytes, and coagulation function, were in normal range. Pituitary
hormone test revealed the thyroid-stimulating hormone (TSH)
of 0.03 mIU/L, adrenocorticotropic hormone (ACTH) of <1 pg/
ml, and free triiodothyronine (fT3) of 2.5 pmol/L. The cortisol,
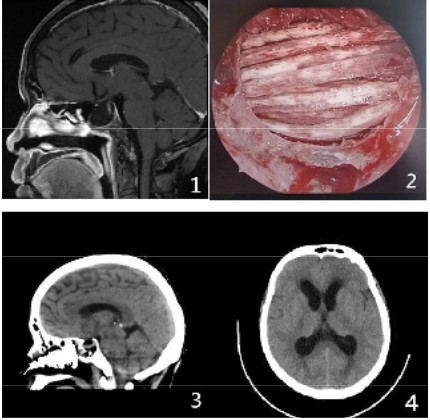
prolactin and growth hormone were in normal range. On cranial MRI, the pituitary fossa enlarged with long signals on T1WI/
T2WI and isointense signal on DWI inside; the pituitary stalk was
shifted towards the right; the optic chiasma was compressed
to elevate; and the bones of the anterior clinoid process (ACP)
and sellar floor got compressed and absorbed. Empty sella was
considered.
Empty sella was diagnosed on admission. After discussion
with the patient and her trustee, elective (right) neuroendoscopic endonasal transsphenoidal surgery under general anaesthesia was performed. The bone of the sellar floor was absorbed and thinned intraoperatively. After grinding, the dura
was exposed as intact and thin. The dura mater was lifted, and
the sella turcica was filled with allogenic bones in a cross-over
fashion. Unfortunately, high-flow cerebrospinal fluid (CSF) leakage occurred intraoperatively due to the rupture of the dura
and was instantly managed using artificial dural patches, fascia
lata from the thign, and fibrine adhesives, etc. The patient was
returned to the ward after surgery and reported improvement
in headache after waking from anaesthesia. However, she complained of visual impairment and could only sense light. No evidence of haemorrhage was revealed on instant cranial CT, and
shock therapy with intravenous Methylprednisolone was ineffective. On day 3 after surgery, the patient developed intracranial infection and was treated by lumbar cistern drainage of CSF
and anti-infective treatment using Vancomycin and Meropenem. Two weeks after surgery, pituitary test revealed the TSH of
0.03 mIU/L and ACTH of <1 pg/ml. Levothyroxine replacement
therapy was performed, resulting in diabetes insipidus which
was then treated by desmopressin acetates. Four weeks after
surgery, the patient had communicating hydrocephalus and
then underwent ventriculoperitoneal shunt. At semi-annual
follow-up, the patient could only identify the number of figures
within a distance of 1 meter.
Discussion
Surgery is not necessary for empty sella patients without significant symptoms or signs. While in patients with intractable
headache, vision loss, visual field defects, hypopituitarism, or
spontaneous CSF rhinorrhoea, surgical intervention is required.
In these cases, surgery is usually performed to fill in the abnormally enlarged subarachnoid space within the sella turcica, removing the compression on the pituitary gland, dura and bone
caused by CSF pulsation, thereby eliminating or reducing the
corresponding symptoms and signs to delay disease progression [3,4].
Empty sella is a medical condition with the sella turcica filled
with CSF. In this context, typical imaging findings of empty sella mainly include punctate signals (pituitary stalk transection)
isointense to the brain tissue on axial image, "White-target
sign" on T2WI, "Black-target sign" on T1WI, and "Funnel sign"
on coronal positions. All these findings have significant value for
diagnosis of empty sella syndrome [5].
Combining the treatment process of the patient reported
here, the preoperative diagnosis of empty sella syndrome was
relatively definitive. Intractable headache has a clear indication
for surgery when drug therapy is ineffective. The patient reported here had CSF leakage during transsphenoidal surgery, resulting in rapid loss of bulk CSF. Besides, the patient also had visual
impairment because of the acute downward herniation of the
optic chiasma due to gravity. According to experience, patients
who have visual impairment after endonasal transsphenoidal
surgery may benefit from the treatment protocol of optic nerve
injury, including early steroid pulse therapy, vasodilator drugs,
and early hyperbaric oxygen therapy. The hypopituitarism after
surgery was considered as a cause of intracranial infection in www.jclinmedsurgery.com 3
this patient. Irrigation of operative field with hydrogen peroxide and iodophors throughout the endonasal transsphenoidal
surgery may reduce the incidence of postoperative intracranial
infection. In addition, tight patching of the dura mater is also
of paramount significance. The patient here had significant
improvement in headache after surgery but developed severe
complications. However, her vision remained severe even after aggressive treatment, which is confusing and upsetting. For
patients suffering from intractable headache, lumbar cistern
drainage of CSF can be performed. While in cases with remission, ventriculoperitoneal drainage can be an option to further
relieve headache [7] and reduce surgery-related trauma.
Conclusion
Here, we describe a rare case of empty sella syndrome with
severe visual impairment occurred postoperatively. The development of visual impairment might be associated with the rapid loss of bulk CSF during surgery. Therefore, it is key to avoid intraoperative loss of bulk CSF that may lead to acute downward
herniation of the optic chiasma. Additionally, tight repair of the
CSF leak with dural patches is vital to prevent the incidence of
postoperative intracranial infection. Here, the patient vision
was not significantly recovered after aggressive treatment, and
we suspected that there might be a close relationship with the
intracranial infection [7].
Declarations
Conflict of interest: All authors state no conflict of interest.
Statement: Informed consent for publication was obtained
from the patient and her surrogates. This case was published
with written informed consent from the patient’s son, which is
a retrospective study and has nothing to do with ethics.
Disclosures: The authors report no conflict of interest in this
paper.
Author contributions
1. Conceptualization: Jingcheng Jiang, Shijun Zhou, Xiaoqin
Qu, LiHua Qiu, Yong Yi
2. Data curation: Jingcheng Jiang, Shijun Zhou,Xiaoqin Qu,
LiHua Qiu, Yong Yi
3. Formal analysis: Jingcheng Jiang
4. Investigation: Jingcheng Jiang
5. Resources: Xiaoqin Qu
6. Supervision: LiHua Qiu, Yong Yi
7. Validation: LiHua Qiu, Yong Yi
8. Writing – original draft: Jingcheng Jiang, Shijun Zhou,
Xiaoqin Qu
9. Writing – review & editing: LiHua Qiu, Yong Yi
References
- Mehla S, Chua AL, Grosberg B, et al. Primary Empty Sella[J].
Headache. 2020 Nov; 60(10): 2522-2525.
- Chiloiro S, Giampietro A, Bianchi A, et al. DIAGNOSIS OF ENDOCRINE DISEASE: Primary empty sella: a comprehensive review[J].
Eur J Endocrinol. 2017 Dec; 177(6): R275-R285.
- Graillon T, Passeri T, Boucekine M, et al Chiasmapexy for secondary empty sella syndrome: diagnostic and therapeutic
considerations[J]. Pituitary. 2021 Apr; 24(2): 292-301.
- Tsukiyama A, Hattori Y, Tahara S, et al. New Technique for Chiasmapexy Using Iliac Crest Bone Graft: 2 Cases of Visual Impairment Caused by Empty Sella Syndrome[J]. World Neurosurg.
2017 Nov; 107: 1051.e19-1051.e25.
- Wang YX,Wan DH, Li ZJ, et al. MRI features of Rathke cleft
cysts with the appearance of mgh density on preoperative CT
image[J]. Chin J Clin Neurosurg. 2022Jan; Vol,27(1): 31-33.
- thy and second optic nerve injuries. JAMA Ophthalmol. 2014
May; 132(5): 567-571.
- Lee TC, Yang LC, Huang PL. Treatment of empty sella syndrome
with ventriculoperitoneal shunt. J Clin Neurosci. 2005 Feb;
12(2): 201-205.
- Ghatalia PA, Vick A, Vattoth S, et al. Reversible blindness in cryptococcal meningitis with normal intracranial pressure: Case report and review of the literature. Clin Infect Dis. 2014 Jul 15;
59(2): 310-313.