Clinical & Medical Surgery
Open Access
Volume 3
Rebeca Tenajas1*; David Miraut2
*Corresponding Author: Rebeca Tenajas
Medical Doctor, Master in Medicina Clínica, Family Medicine Department, Arroyomolinos Community Health Centre, Spain.
Email: rebeca.tenajas@salud.madrid.org
Article Info
Received: May 16, 2023
Accepted: Jun 12, 2023
Published: Jun 19, 2023
Archived: www.jclinmedsurgery.com
Copyright: © Tenajas R (2023).
Abstract...
This article presents a rare case of Trigonum Bone Syndrome in an 8-year-old girl, diagnosed using X-ray, Computed Tomography (CT) and contrast-enhanced magnetic resonance imaging (MRI). The patient presented persistent ankle pain and ligamentous distention, not responding to conservative treatments. Surgical removal of the accessory bone and subsequent rehabilitation led to successful outcomes
Citation: Tenajas R, Miraut D. Clinical Presentation and Management of Trigonum Bone Syndrome in a Pediatric Patient. J Clin Med Surgery. 2023; 3(1): 1103.
Introduction
Trigonum Bone Syndrome, also known as ‘os trigonum syndrome’, is a rare condition characterized by the presence of an accessory bone in the talus (astragalus). This additional bone, the os trigonum, can cause pain, swelling, and reduced range of motion in the affected ankle joint. The etiology of the condition is believed to be congenital, arising from the non-fusion of an accessory ossification center during embryological development [1]. The incidence of os trigonum is reported to be below 7% of the general population, though symptomatic cases are rare [2], although relatively prevalent in elite ballet dancers and athletes [3,4].
Case presentation
An otherwise healthy 8-year-old school girl visited the Community Health Centre with a complaint of localized pain in her right ankle, which had been persisting for several weeks. The pain was associated with ligamentous distention and was exacerbated during physical activities. She had a history of frequent ankle joint pain, which had not responded to functional bandages or physiotherapy. A clinical examination revealed localized tenderness and mild swelling over the posterolateral aspect of the ankle, with no signs of infection or systemic illness.
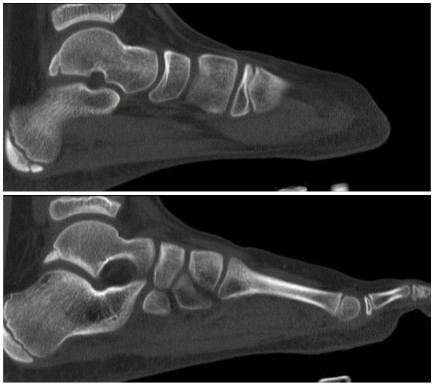
A weight-bearing anteroposterior (AP) and lateral X-ray of the right ankle were performed, revealing an accessory bone within the talus. The os trigonum was well-corticated and situated at the posterior aspect of the talus, adjacent to the talocalcaneal joint (Figure 1). The differential diagnosis at this stage included an ununited fracture fragment, osteochondroma, and os trigonum.
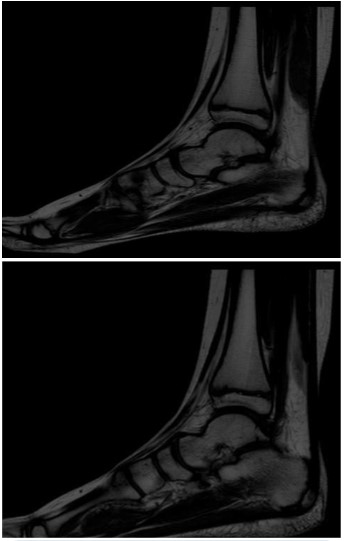
To further assess the nature of the accessory bone and to delineate the soft tissue involvement, both a CT and a contrast-enhanced MRI of the right ankle was performed. The CT confirmed the presence of an os trigonum (Figure 2), and the MRI provided the evidences of adjacent soft tissue edema and inflammation, suggesting the presence of Trigonum Bone Syndrome (Figure 3). There was no evidence of osteochondral lesions or other bony abnormalities.
After discussing the available treatment options with the patient’s parents, the decision was made to proceed with surgical intervention. The patient was admitted for an excision of the os trigonum and exploration of the surrounding soft tissue structures. The surgery was performed under general anesthesia, with the patient in a prone position. A posterolateral approach to the ankle joint was utilized, with careful dissection of the soft tissues to protect the neurovascular structures. The os trigonum was identified, and its fibrous attachments to the talus were released. The accessory bone was then excised, and the surrounding soft tissues were carefully inspected for any signs of injury or inflammation. The wound was closed in layers, and a sterile dressing was applied.
Postoperative recovery was uneventful, with the patient experiencing significant pain relief and improved range of motion in her right ankle. She was referred for rehabilitation, which included a gradual return to weight-bearing activities and a tailored physiotherapy program to strengthen the surrounding musculature and improve joint stability.
Discussion
Trigonum Bone Syndrome is a rare condition that occurs due to the presence of an accessory bone, the os trigonum, in the talus. The presence of this extra bone can lead to discomfort, pain, inflammation, and limited mobility in the ankle joint that is affected. Although the presence of an os trigonum is relatively common, symptomatic cases are rare and often require surgical intervention [5].
The etiology of Trigonum Bone Syndrome is thought to be congenital, arising from the non-fusion of an accessory ossification center during embryological development [1]. The ossification center for the os trigonum appears around the 10th week of gestation and typically fuses with the primary ossification center by the age of 8 to 13 years [2]. Failure of this fusion process results in the presence of an os trigonum.
Diagnosis of Trigonum Bone Syndrome can be challenging due to its rarity and non-specific clinical presentation. In this case, the initial diagnosis was made using plain radiographs, which showed the presence of an accessory bone in the talus. Further evaluation using a CT and a contrast-enhanced MRI helped to confirm the diagnosis and assess the extent of soft tissue involvement [6]. The findings of Magnetic Resonance (MR) imaging include edema in the talus and/or os trigonum, fluid in the synchondrosis, fluid surrounding the os trigonum, and alterations in soft tissue. Additionally, MR can reveal related findings such as stenosing tenosynovitis of the flexor hallucis longus and degenerative changes around the synchondrosis or between the os trigonum and the adjacent calcaneus.
Treatment options for Trigonum Bone Syndrome vary depending on the severity of the symptoms and the extent of soft tissue involvement. Conservative measures, such as rest, ice, compression, elevation, and analgesics, are often recommended initially [7]. In cases where these measures fail to provide adequate relief, as in our patient, surgical intervention may be necessary.
Several surgical approaches have been described for the excision of the os trigonum, including open and arthroscopic techniques [8]. In this case, an open posterolateral approach was utilized, which allowed for direct visualization of the os trigonum and the surrounding soft tissue structures. The choice of surgical approach should be based on the surgeon's familiarity with the technique, the patient's anatomy, and the extent of soft tissue involvement.
Postoperative management typically involves a period of immobilization followed by a gradual return to weight-bearing activities and a tailored physiotherapy program. In our patient, the postoperative recovery was uneventful, with significant improvement in pain and range of motion in the right ankle. This highlights the importance of early diagnosis and appropriate surgical intervention in achieving successful outcomes in patients with Trigonum Bone Syndrome.
In light of the rarity of Trigonum Bone Syndrome, increased awareness among clinicians and surgeons is essential. Early diagnosis and appropriate management can significantly improve patient outcomes and prevent potential complications, such as chronic pain, instability, or reduced range of motion. Furthermore, understanding the embryological basis of this condition can contribute to the development of more targeted and effective treatments in the future.
It is important to note that while our case report focuses on a pediatric patient, Trigonum Bone Syndrome can affect individuals of all ages. In particular, it has been reported in athletes who engage in repetitive plantarflexion activities, such as ballet dancers and soccer players [4,3]. In these populations, early recognition and treatment are crucial to avoid potential longterm consequences and to facilitate a safe and timely return to sports.
Additionally, clinicians should be aware of the potential differential diagnoses when encountering a patient with posterior ankle pain and an accessory bone in the talus. These may include conditions such as an ununited fracture fragment, osteochondroma, or a Stieda process [5]. Careful evaluation of the patient's history, clinical presentation, and imaging findings can help to differentiate these entities and guide appropriate management.
Lastly, this case report highlights the role of advanced imaging techniques, such as CT and contrast-enhanced MRI, in the diagnosis and management of Trigonum Bone Syndrome. As the condition is characterized by the involvement of both osseous and soft tissue structures, the use of MRI can provide valuable information on the extent of the pathology and aid in surgical planning [3].
Trigonum Bone Syndrome is an unusual but important cause of posterior ankle pain, particularly in pediatric patients and athletes. Early diagnosis and appropriate management, including surgical intervention when necessary, can lead to successful outcomes and prevent long-term complications. Clinicians and surgeons should maintain a high index of suspicion for this condition and be familiar with its diagnostic and treatment options. Further research is needed to improve our understanding of the etiology, natural history, and optimal management strategies for this rare condition.
Conclusion
Trigonum Bone Syndrome is an uncommon condition identified by the existence of an accessory bone within the talus. This can cause discomfort, pain, inflammation, and diminished mobility in the ankle joint that is affected. The diagnosis can be challenging due to its rarity and non-specific clinical presentation, but imaging studies such as X-ray, CT and contrast-enhanced MRI can aid in the diagnostic process. Surgical intervention is often necessary in cases where conservative measures fail to provide adequate relief. In this case, surgical excision of the os trigonum and subsequent rehabilitation led to a successful outcome, highlighting the importance of early diagnosis and appropriate management in patients with this rare condition
Declarations
Conflict of interest: None reported.
Funding sources: The authors received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments: We thank the parents’ patient for granting permission to publish the clinical images.
References
- Sarrafian SK. Anatomy of the foot and ankle: descriptive, topographic, functional. 3rd edn.. Lippincott Williams & Wilkins. 2011.
- Kalantari BN, Seeger LL, Motamedi K, Chow K. Accessory ossicles and sesamoid bones: spectrum of pathology and imaging evaluation. Applied Radiology. 2007; 36: 28.
- Baillie P, Cook J, Ferrar K, Smith P, Lam J, et al. Magnetic resonance imaging findings associated with posterior ankle impingement syndrome are prevalent in elite ballet dancers and athletes. Skeletal Radiology. 2021; 50: 2423-2431.
- Abramowitz Y, Wollstein R, Barzilay Y, London E, Matan Y, Shabat S, et al. Outcome of resection of a symptomatic os trigonum. J Bone Joint Surg Am. 2003; 85-A: 1051-1057.
- Keles-Celik N, Kose O, Sekerci R, Aytac G, Turan A and Guler F. Accessory Ossicles of the Foot and Ankle: Disorders and a Review of the Literature. Cureus. 2017; 9. e1881. 10.7759/cureus.1881.
- Karasick D, Schweitzer ME. The os trigonum syndrome: imaging features. AJR. American Journal of Roentgenology. 1996; 166: 125-129.
- Safer VB, Safer U, Kaya L. An Unusual Os Trigonum Syndrome Case Secondary to Car Accident: A Case Report. Middle East J Rehabil Health. 2016; 3: e36719.
- Ahn JH, Kim YC, Kim HY. Arthroscopic versus posterior endoscopic excision of a symptomatic os trigonum: a retrospective cohort study. Am J Sports Med. 2013; 41: 1082-1089.