Clinical & Medical Surgery
Open Access
Volume 3
*Corresponding Author: Hajer Touil
Department of Oral and Maxillo-Facial Surgery, University Hospital of Mahdia, Tunisia.
Email: hajer.touil@yahoo.com
Article Info
Received: May 04, 2023
Accepted: Jun 02, 2023
Published: Jun 09, 2023
Archived: www.jclinmedsurgery.com
Copyright: © Touil H (2023).
Abstract...
Introduction: Herpes zoster of the mandibular branch of the trigeminal nerve is a disease that often challenges oral and maxillo-facial surgeons and dentists trying to make the proper diagnosis. Therefore, the objective of this report is to present a brief review of herpes zoster infection involving the mandibular branch of the trigeminal nerve, treatment modality and diagnostic considerations.
Case Report: We report a clinical case in which a 72-year-old woman sought care for a vesicular lesion along the left mandibular area.
Discussion: Herpes zoster is an acute neurodermic viral infection that occurs during the lifetime of about 10-20% individuals. Reactivation occurs in 30% of infected individuals resulting in herpes zoster with characteristic dermatome distribution. The branch of the trigeminal nerve which is most often affected is the ophthalmic nerve. Mandibular nerve involvement is much rarer. Early prescription of antiviral agents hastens acute symptoms’ resolution and possibly decreases the risk of postherpetic neuralgia.
Conclusion: Clinicians should understand that when herpes zoster involves the mandibular branch, it can appear in the presence or absence of skin lesions, its diagnosis might be difficult for clinicians. It must be established before any invasive treatment. Early initiation of antiviral treatment accelerates recovery and may decrease the risk of postherpetic neuralgia.
Citation: Touil H. Involvement of Herpes Zoster in the Mandibular Branch of the Trigeminal Nerve: A New Case Report. J Clin Med Surgery. 2023; 3(1): 1101.
Introduction
Herpes zoster also known as shingles, occurs when the varicella zoster virus, which causes both varicella and herpes zoster, is reactivated from its latent state in the dorsal root or cranial nerve ganglia and spreads through the afferent nerve to the skin. Atypical presentations may be challenging to praticians. Reactivation symptoms commonly affect the thoracolumbar trunk, and rarely affect the mandibular branches of the trigeminal nerve [1].
Herein, we report a new case of a Herpes zoster infection that involved the mandibular branch of the trigeminal nerve.
Case report
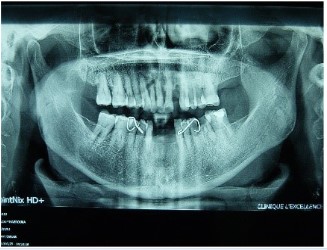
A 72-year-old woman with a history of diabetes on oral antidiabetics and parkinson’s disease on parkisol, consulted the department of Oral and Maxillofacial surgery of the university Hospital of Mahdia, and her chief complaint was an erythematous maculopapular itchy rash along the left mandibular area which was followed by the appearance of clear vesicles for 4-6 days and subsequent pustulation and scabbing (Figure 1). The patient also suffered at first from hemimandibular pain described as burning sensation that she neglected. Intraoral examination didn’t show alveolar exposure or tooth mobility, besides, there were no abscesses from her dentition. Physical examination revealed no lymphadenopathy or other affected areas, and the patient was afebrile. Panoramic view showed no abnormal anomalies (Figure 2). In front of the typical presentation (painful lesion, unilateral, not crossing the midline skin rash, dermatomal) and the chronological skin changes (prodromal pain followed by blisters then crusts after fluid dried), we diagnosed her condition as a left trigeminal herpes zoster. We prescribed acyclovir and pregabalin. The favorable response to this treatment confirmed the diagnosis. No tooth loss, bone exposure, or osteonecrosis occurred during the follow-up period. Also, no other complications, such as postherpetic neuralgia, occurred.
Discussion
Herpes zoster virus (HZV) is reponsable for both varicella and herpes zoster [2]. After primary infection, the virus remains latent in the sensory ganglia probably for the remaining host’s life. Reactivation of HZV may occur spontaneously or when host defences are compromised. Predisposing factors can be physical trauma (including dental procedures), psychological and surgical stress, malignancy, radiation therapy and immunocompromised states including transplant recipients, steroid therapy and HIV infection and increased age [3,4]. In fact, it reacti- vates most commonly in persons older than 50 years who have agerelated weakening of the immune system [1,4,5]. Therefore, prompt management is necessary to avoid morbidity and mortality in these individuals [3]. The infection, is reponsable for radiculoneuritis. In fact, it is characterized by a bandlike rash in the dermatome that corresponds to the affected nerve [3,5].
The facial involvement usually includes the ophthalmic branch of the trigeminal nerve [5]. The involvement of mandibular branch is comparatively rare [3,6]. It may be accompanied by mucosal lesions and dental complications such as devitalized teeth, internal resorption and spontaneous exfoliation of the teeth [5]. In these cases, the symptomatology is charaterized by toothache which often precedes the icthy rash, making early diagnosis difficult [6].
The common timeline for shingles is to 3 to 5 days of prodromal phase, followed by a 5-days-eruption of vesicules or blisters that dry and form crust after liquid secretion. Complete healing typically takes 2 to 4 other weeks. But in many instances, resolution can take much longuer. The pain associated with shingles varies in intensity from mild to severe in such a way that even the slightest stimuli can elicit excruciating spasms [3].
The chronic pain syndrome stage, termed postherpetic neuralgia, has been described as pain lasting 1 to 3 months after the skin lesions have cleared, but may last for years and decades, becoming a significant cause of morbidity [3].
Early diagnosis and appropriate treatment are crucial to prevent this condition, cause once it occurs, there are no real effective treatment. Recently, the use of antidepressive therapy and neurolyptics in the management of this complication was described [6].
Besides, when there is maxillary or mandibular involvement, more specific complications, such as alveolar bone necrosis or tooth exfoliation, are reported to occur.
Bone necrosis may appear between 9 and 150 days after the onset of shingles, with an average of 30 days with an infection most often severe. This variable time may, therefore, justify the regular and prolonged follow-up for several months of these at-risk patients [5].
The differential diagnosis, difficult in the pre-eruptive phase, arises during the rash with acute superinfected osteitis. The panoramic X-ray image eliminates this pathology.
Although it is a self-limiting disease, early institution of antiviral treatment and symptomatic therapy reduces the morbidity significantly. Multiple randomized, controlled trials found that oral acyclovir (800 mg 5 times a day for 7 days), famciclovir (500 mg every 8 hours for 7 days) and valacyclovir (1000 mg 3 times a day for 7 days) associated to an analgesic treatment reduce acute pain and duration of chronic pain in older herpes zoster patients who are treated within 72 hours of rash onset [3].
Conclusion
Making the diagnosis of mandibular nerve shingles can be quite challenging, especially in the absence of typical rash. This is why it is necessary to always think of the mandibular herpes zoster in front of toothache, vesicles and ulcerations on the movable or non-movable oral mucosae especially when they precede a unilateral, dermatomal skin rash and do not progress favorably under antibiotic treatment.
References
- Meer S, Coleman H, Altini M, Alexander T. Mandibular osteomyelitis and tooth exfoliation following zoster-CMV co-infection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101: 70-5.
- Rudd T, Chai BY, Glasgow M, Gurunluoglu R. Mandibular Osteonecrosis and Ramsay Hunt Syndrome following a case of Herpes Zoster. J Oral Maxillofac Surg. 2014; 72: 1974.e1-6.
- Nair P, Gharote H, Singh P, Jain-Choudhary P. Herpes zoster on the face in the elderly. BMJ Case Rep. 2014; 2014: bcr2013200101.
- Thada SR, Gadda R, Pai K. Nerve afflictions of maxillofacial region: A report of two cases. BMJ Case Rep. 2013.
- Faure E, Engels-Deutsch M, Paraschiv EA, Gérard, Curien R. Mandibular osteonecrosis following herpes zoster infection : Report of a rare case with a literature review. Clin Case Rep. 2021; 9: e04196.
- Yang SH, Jung DH, Lee HD, Lee Y, Chang HS, et al. Clinical Diagnosis of Herpes Zoster Presenting as Odontogenic Pain. J Kor Acad Cons Dent. 2008; 33: 452-456.