Clinical & Medical Surgery
Open Access
Volume 3
Libo Jin1; Hang Zhang2; Junqing Zhou1; Haixia Xu1*
*Corresponding Author: Haixia Xu
Department of Cardiovascular Surgery, Shaoxing People’s Hospital, Shaoxing, China.
Email: 601525107@qq.com
Article Info
Received: Apr 03, 2023
Accepted: Apr 27, 2023
Published: May 04, 2023
Archived: www.jclinmedsurgery.com
Copyright: © Xu H (2023).
Abstract...
Background: Ascending aortic thrombosis is extremely rare and its pathogenesis is unclear. Clinical manifestations are often related to the site of embolism caused by thrombus dislodgement. Currently, surgery is considered the first choice to prevent embolism and recurrence, while medical therapy is an option for patients who refuse surgery or for whom surgery is contraindicated.
Case presentation: We present a case of myocardial infarction caused by a dislodged thrombus in the ascending aorta. The patient refused surgery and requested conservative treatment. After anticoagulation, the patient improved and was discharged from the hospital.
Conclusion: Because of its rarity, the pathogenesis and treatment of aortic thrombosis are unclear. Artery CT (CTA) is recommended as the first choice because of its convenience and high sensitivity, and surgery is considered the best way to eradicate thrombosis and prevent recurrence.
Citation: Jin L, Zhang H, Zhou J, Xu H. A Case Report of Myocardial Infarction due to a Dislodged Thrombus in the Ascending Aorta. J Clin Med Surgery. 2023; 3(1): 1091.
Introduction
Ascending aortic thrombosis is extremely rare and its pathogenesis is unclear. Clinical manifestations are often related to the site of embolism caused by thrombus dislodgement. Here, we present a case of myocardial infarction caused by a dislodged thrombus in the ascending aorta to raise awareness of the diagnosis and treatment of this condition.
Case presentation
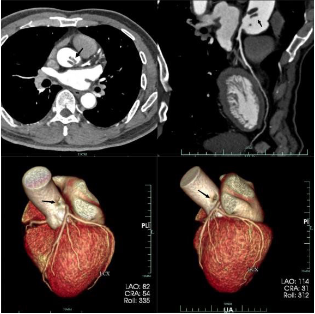
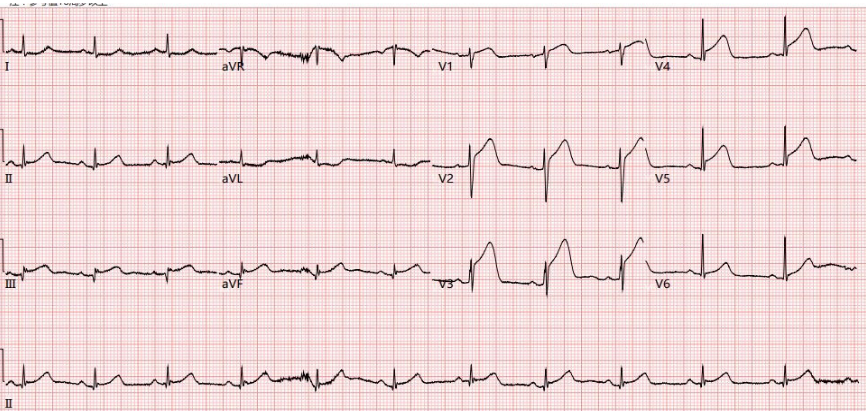
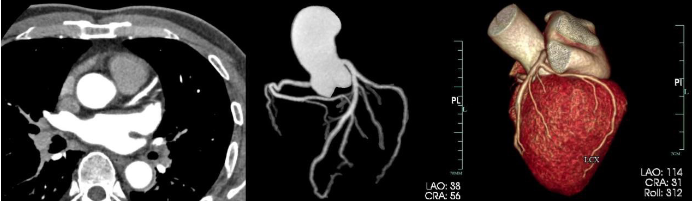
The patient, a 58-year-old man, was admitted to the hospital for half a day for chest pain. He had hypertension and a long history of smoking. Physical examination: No obvious dry or wet rales were heard in either lung, the heart rhythm was regular, and no obvious murmur was heard on auscultation of the heart. On admission, troponin was normal and the Electrocardiogram (ECG) showed sinus rhythm and mild ST changes. To exclude myocardial infarction, we performed a coronary CT, which revealed no significant stenosis of the coronary arteries. Instead, there was an abnormal filling defect at the beginning of the ascending aorta, close to the orifice of the left coronary artery, and a thrombus was considered (Figure 1). We recommended surgery, but the patient declined, strongly urging pharmacological treatment. During anticoagulation therapy, the patient developed recurrent chest pain and blood tests revealed elevated troponin (23.82 ng/ml, U L N<1 ng/ml) and an ECG suggestive of V1-5, II, III, aVF ST elevation (Figure 2). Ultrasound showed reduced myocardial activity in the left anterior and anterior interventricular walls, EF: 55%. The clinical diagnosis suggested a myocardial infarction. However, the patient insisted on conservative treatment and was therefore given aspirin and clopidogrel for antiplatelet aggregation and heparin for anticoagulation. After one week of treatment, the patient’s serum troponin gradually decreased, and a repeat coronary CT showed no significant abnormalities in the coronary arteries and disappearance of the ascending aortic thrombus (Figure 3).
Discussion and conclusions
Aortic thrombosis is clinically rare. It occurs mainly in the abdominal aorta and rarely in the ascending aorta [1]. Due to its fast flow and high pressure, the ascending aorta is generally not prone to thrombosis. The mechanism of aortic thrombosis is unclear and may be related to atherosclerosis, aortic ulcer formation, aortitis, aortic aneurysm, hematologic disorders (e.g., protein S or protein C deficiency and antiphospholipid antibody syndrome), and long-term hormone use causing blood hyper-coagulation [2,3]. In this case, the patient had a history of hypertension and long-term smoking, and CTA revealed localized irregular depression at the beginning of the ascending aorta, so we presume that the thrombus was formed on the basis of focal atherosclerosis of the aorta.
The clinical symptoms of aortic thrombosis are atypical and are easily overlooked and misdiagnosed in the early stages. It is not recognized until the thrombus is dislodged and causes organ embolism, so the prognosis is often poor. A meta-analysis of 200 patients with symptomatic aortic thrombosis found that acute arterial ischemia of lower limbs was the most common embolism manifestation (84%), followed by visceral ischemia (27%) and stroke (14%) [4]. Due to the high risk of aortic thrombosis, early detection and treatment are particularly important. CTA is recommended as the test of choice because of its convenience and high sensitivity [5]. Transthoracic or transesophageal echocardiography is also highly accurate and can be used to assess the size, shape, location of attachment and aortic wall characteristics of thrombi located in the proximal ascending aorta [6].
There is little national and international literature on aortic thrombosis, and there are no guidelines to follow for treatment. The main treatment modalities are anticoagulation, thrombolysis, surgery, etc. Although there have been cases of good results with conservative medication, surgical resection is still considered the best way to eradicate thrombosis and prevent recurrence [7,8]. On the one hand, drug anticoagulation, thrombolysis, and other treatments have the potential for non-dissolution or incomplete dissolution of the thrombus; on the other hand, there is a risk of peripheral vascular embolism caused by dislodged thrombus during the treatment process [9]. In the meta-analysis of 98 articles included by Fayad et al., 112 patients received anticoagulation therapy while 88 patients received aortic surgery. Patients who received anticoagulation had a higher rate of peripheral arterial embolism and thrombotic recurrence than those who underwent surgery [4]. Therefore, medical therapy is often indicated for patients who have difficulty tolerating or refusing surgery. The patient in this case refused surgery and requested conservative treatment. Myocardial infarction was caused by a dislodged aortic thrombus during drug treatment, so we administered anticoagulation and antiplatelet therapy. One week after treatment, a repeat CTA revealed complete dissolution of the thrombus.
Declarations
Ethics approval and consent to participate: The present study was approved by the Ethics Committee of Shaoxing People’s Hospital (Shaoxing, China). Written informed consent was obtained from the patient.
Patient consent for publication: Written informed consent for the publication of clinical details and images was obtained from the patient.
Availability of data and materials: Data are available upon request.
Competing interests: Not applicable.
Funding: None.
Acknowledgements: Not applicable.
References
- Teranishi H, Tsubota H, Arai Y and Hanyu M. Floating thrombus in the ascending aorta. Journal of cardiac surgery. 2016; 31: 549-550.
- Yamase Y, Kuwabara F, Watanabe K, Yajima K, Akita N, et al. A case of floating thrombus in the ascending aorta that caused recurrent peripheral arterial embolic events. J Cardiol Cases. 2015; 12: 57-60.
- Weiss S, Bühlmann R, von Allmen RS, Makaloski V, Carrel TP, et al. Management of floating thrombus in the aortic arch. J Thorac Cardiovasc Surg. 2016; 152: 810-817.
- Fayad ZY, Semaan E, Fahoum B, Briggs M, Tortolani A, et al. Aortic mural thrombus in the normal or minimally atherosclerotic aorta. Ann Vasc Surg. 2013; 27: 282-290.
- Wang B, Ma D, Cao D and Man X. Huge thrombus in the ascending aorta: a case report and literature review. J Cardiothorac Surg. 2019; 14: 157.
- Yang P, Li Y, Huang Y, Lu C, Liang W and Hu J. A giant floating thrombus in the ascending aorta: a case report. BMC Surg. 2020; 20: 321.
- Iosifescu AG, Radu C, Marin SL and Enache R. Floating thrombus of the ascending aorta after treatment of ureteral carcinoma: A case report. Turk Gogus Kalp Damar Cerrahisi Derg. 2022; 30: 444-447.
- Toyama M, Nakayama M, Hasegawa M, Yuasa T, Sato B, et al. Direct oral anticoagulant therapy as an alternative to surgery for the treatment of a patient with a floating thrombus in the ascending aorta and pulmonary embolism. J Vasc Surg Cases Innov Tech. 2018; 4:170-172.
- Sosa C and Zuccarino F. Floating Aortic Thrombus in a Non-aneurysmal and Non-atherosclerotic Aorta. Eur J Vasc Endovasc Surg. 2018; 55: 491.