Introduction
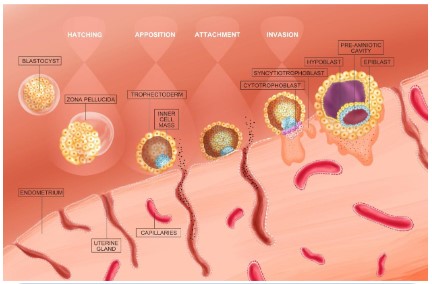
Successful implantation of the embryo requires appropriate
embryonic development and also requires that the mother has
a well-conditioned endometrium. In humans, the uterus becomes receptive to implantation in the mid-luteal phase of the
menstrual cycle, which is often referred to as the window of implantation. Implantation is a complex process that is subject to
complex molecular regulatory mechanisms such as hormones,
growth factors and cytokines (Figure 1). The initial step of the
implantation process is the apposition and contact of the blastocyst with the endometrial epithelium, followed by the invasive activity of trophoblast cells between the epithelial cells. It
has been reported in the literature that inadequate tolerance
of the uterus will lead to about half of the implantations are
abnormal and pregnancy failure [1-3]. Although assisted reproductive technologies have helped humans overcome most infertility problems, successful embryo implantation remains an
important step for successful in vitro fertilization.
The endometrium is composed of two cellular components,
namely surface epithelial cells and mesenchymal cells. The endometrium is not stable and unchanging, but is a dynamic tissue that undergoes several changes during the menstrual cycle
including morphological histology, biochemistry and molecular
biology, which are essential elements for a successful embryo
implantation process. Estrogen and progesterone stimulate the
endometrium, with estrogen causing proliferation and thickening of the endometrium, and progesterone causing secretory
changes, metaplasia, puffiness and thickening of the endometrium. Together, these two hormones promote the growth of
the endometrium and induce differentiation of endometrial
mesenchymal cells into metaphase, which ultimately provides
an acceptable site for implantation of the blastocyst.
In assisted reproductive techniques, the development of
the mother’s endometrium is usually observed by transvaginal ultrasound. An accepted marker of uterine capacitance is
the thickness of the endometrium [4]. For successful embryo
transfer, the recommended minimum endometrial thickness is
7 mm, even though there is no standard value for diagnosing
a thin endometrium [5]. In addition, higher implantation rates
can be achieved with endometrial thicknesses greater than 9
mm. In contrast, a persistently thinner endometrium may be
associated with a lower rate of implantation as well as a higher
rate of miscarriage [6]. Therefore, many researchers around
the world have tried to find some treatments that can improve
endometrial tolerance and endometrial thickness. Although
several treatments have been tried clinically (granulocyte colony-stimulating factor, sildenafil, low-dose aspirin, stem cell
therapy, acupuncture, and physical therapy), clinical outcomes
have been inconclusive. In this review, we review the literature
on thin endometrium and discuss recent therapeutic tools and
recent progress of thin endometrium to inform clinicians on
better treatment options.
Granulocyte colony-stimulating factor (G-CSF)
G-CSF is a hematopoietic growth factor, a factor that has positive effects on non-hematopoietic cells, including the endometrium [7]. In a prospective cohort study conducted by Gleicher
et al. in 2011, the authors’ team used G-CSF for transvaginal
endometrial perfusion to treat thin endometrium. The results
showed that four patients previously resistant to estrogen and
vasodilator therapy had successful endometrial expansion to
a minimum thickness of at least 7 mm after uterine perfusion
with G-CSF, suggesting that intrauterine G-CSF may have a direct role in promoting endometrial growth [8]. A preliminary
cohort study [9] showed an increase in endometrial thickness
from 6.4 mm to 9.3 mm (P < 0.001) at an interval of 5.2 days
between G-CSF infusion and embryo transfer. The mean change
was 2.9 mm and did not change between conception and non-conception cycles. This is sufficient to demonstrate the utility of
G-CSF in the treatment of chronic thin endometrium and that
this treatment would result in a good overall clinical pregnancy
rate (19.1%). Lucena et al[10] found that uterine infusion of G-CSF rapidly increased the thickness of the endometrium, thus
ensuring a higher chance of successful pregnancy and a healthy
birth rate of the baby. These results suggest that G-CSF is a factor involved in endometrial remodeling, which enhances the
synchronization between the uterine environment and embryonic development.
Li et al [11] evaluated the effectiveness of G-CSF in a frozen
embryo transfer program for infertile women with thin endometrium. The G-CSF group had a higher rate of induced cycles
and a lower rate of natural cycles compared to the control group
and showed a trend towards better implantation and clinical
pregnancy rates. Similarly, Kunicki et al. reached similar conclusions [12]. Kunicki’s team did a follow-up visit of 37 subjects
with thin and unresponsive endometrium on the day of ovulation triggering. In all subjects, endometrial thickness was 6.74
mm beofre G-CSF infusion and increased significantly to 8.42
mm after infusion [12]. In another non-randomized interventional clinical trial, Eftekhar et al [13] compared the effects of
in utero G-CSF treatment and direct embryo transfer in patients
with endometrium (<7 mm). All patients were treated with
oral estradiol and transvaginal sildenafil and on day 12 or 13,
patients in the G-CSF group would receive intrauterine G-CSF
therapy. While this study failed to demonstrate the potential
of G-CSF to improve endometrial thickness, G-CSF treatment
has the potential to improve clinical pregnancy rates in infertile
women with thin endometrium in frozen-thaw embryo transfer
cycles. Tehraninejad et al [14] performed intrauterine G-CSF infusion in 15 patients who underwent embryo transfer and were
cancelled due to thin endometrium. The endometrial thickness
of these patients increased from 3.59 mm to 7.120 mm with a
clinical pregnancy rate of 20%.
However, negative results were also obtained by some research teams. Barad et al [15] conducted a randomized parallel double-blind controlled clinical trial to determine whether
G-CSG affects endometrial thickness, implantation rate and
clinical pregnancy rate. The results showed no statistically significant difference in increased endometrial thickness between
the G-CSF group and the control group. However, this study was
obtained in an older patient population, so they may not necessarily be applicable to younger women. In another prospective
study, Miralaei et al [16] found a significant change in endometrial thickness after G-CSF treatment (p<0.001); however, nine
patients (45%) did not reach an endometrial thickness of 7 mm
and therefore the embryo transfer was cancelled. The above
evidence allows people to know that although intrauterine infusion of G-CSF has a potential role in increasing endometrial
thickness in patients, the rate of transfer failure remains high
and events of poor pregnancy outcome are observed.
In 2016, Lee and his team explored the efficacy of intrauterine infusion of G-CSF in infertile women with thin endometrium
on trigger day or the day of egg retrieval [17]. The overall clinical pregnancy rate was 22.0%, the implantation rate was 15.9%,
and the ongoing pregnancy rate was 20%. Interestingly, there
was a trend towards higher implantation, clinical pregnancy
rates and sustained pregnancy rates with G-CSF infusion on the
trigger day [17]. This provides a clinical rationale for the timing
of intrauterine G-CSF infusion.
Stem cell therapy
Among many types of cellular therapies, stem cell therapy is
considered to be an effective treatment [18]. Stem cells are capable of differentiating into pluripotent stem cells, and several
studies have been conducted to enumerate the advantages and
disadvantages associated with stem cell therapy [19]. A recent
review published in the journal Cell in 2021 writes that stem cells are now increasingly considered as promising alternative
therapies for translational research in regenerative medicine.
Considering the less ethical issues and easy access to abundant
resources, induced pluripotent stem cells and mesenchymal
stem cells have been extensively studied within the field of infertility to understand their potential applications in reproductive medicine.
Similar to most treatments, stem cell therapy can come with
side effects. For example, before stem cells are used, they are
harvested from embryos and cultured for several months. When
stem cells are harvested from the adult body, especially from
the bone marrow, it can put the patient through many painful
procedures. In addition, stem cell therapy has the potential to
cause a certain percentage of rejection [20].
Mesenchymal stem cells
MSCs are adult stem cells that can be obtained from a variety
of tissues, including bone marrow, umbilical cords, menstrual
blood, endometrial tissue, and adipose tissue. Given their ability to self-renew and differentiate, MSCs are considered by some
studies to be the most attractive cell therapy candidates in regenerative medicine [21]. This property can reflect the origin of
the tissue, as MSCs isolated from different tissues show different sensitivities to inducible bioactive molecules in the culture
medium. A well-known example is adult bone marrow-derived
MSCs, which are often used as the standard type of MSCs. The
conditions of induction of bone marrow-derived MSCs differ
from those of adipose-derived MSCs, which may be attributed
to the existence of a different microenvironment in the vascular system where the cells are located [22]. In addition, several
in vitro experiments have demonstrated the excellent in vitro
regenerative potential of MSCs. The protective role played by
bone marrow MSCs after allogeneic transplantation has been
reported in several models of injury, such as damaged nerve,
myocardium, liver, cartilage and bone tissue, among others [23].
It is currently believed that the therapeutic effects of MSCs
are mainly due to their immunomodulatory function, which is
associated with anti-inflammatory effects through the regulation of the adaptive and innate immune system lymphocytes.
In addition, MSCs have been shown to modulate the immune
response in a variety of diseases [24]. Besides, MSCs are able
to regulate T cell function and proliferation, balance Th2 and
Th1 activity, upregulate Tregs function, inhibit B and NK cell
function, and prevent dendritic cell activation and maturation
[25]. Additionally, MSCs stimulate the proliferation and cytokine secretion of innate lymph-like cells, a new family of lymph like cells that play an important role in innate defense against
pathogens.
The effectiveness of MSCs in treating thin endometrium has
also been confirmed by several studies. Zhao et al [26] established a rat model of thin endometrium by injecting ethanol
into the uterine cavity in order to investigate whether direct
transplantation of MSCs into the uterine cavity could improve
endometrial thickness. The results showed that the endometrium of rats in the intrauterine cavity transplanted with MSCs
group was significantly thickened, and the expression of cytokeratin, wave protein, integrin αγβ3 and leukemia inhibitory
factor was higher than that of the control group. The expression of some pro-inflammatory cytokines such as tumor necrosis factor and interleukin 1 was significantly downregulated,
while the expression of anti-inflammatory cytokines such as
basic fibroblast growth factor and interleukin 6 was significantly upregulated. The authors concluded that uterine perfusion of
MSCs represents a promising new therapeutic tool to address
the currently intractable problem of endometrial thinning. In
another study, Jing and his team explored whether bone marrow MSC treatment could promote endometrial regeneration
and improve endometrial tolerance [27]. They implemented
a randomized controlled animal study in which bone marrow
MSC transplantation was performed by tail vein injection. The
results showed that the endometrium of the experimental
group was significantly thickened and the expression of cytokeratin, wave protein, integrin αγβ3, and leukemia inhibitory factor
was significantly enhanced compared to the control group. The
above evidence could suggest that MSCs are beneficial to thin
endometrium, which may act through the migration and immunomodulation of MSCs.
Mesenchymal stem cell-derived extracellular vesicles
(MSC-EVS)
Recent studies have also focused on the study of exosomes
secreted by mesenchymal stem cells. Exosomes are active paracrine components with a high potential to repair damaged tissues. Exosomes include many paracrine factors responsible for
regeneration and angiogenesis [28]. MSC-EVS is a lipid bilayer
complex that acts as a mediator by transferring multiple molecules (e.g., proteins, microRNAs, lipids, and cytokines) to the recipient cells. The basic mechanisms of action of MSC-EVS have
been agreed upon and include promotion of angiogenesis, anti-fibrosis, immunomodulation and anti-oxidative stress levels.
However, many issues need to be fully substantiated before
MSC-EVS can be used in the clinic, including standardized purification and identification methods, suitable storage and transport systems, large-scale production facilities, and safety issues.
In addition, limited yield is one of the major issues limiting the
widespread use of MSC-EVS. Overall, MSC-EVS shows great potential in regenerative medicine compared to MSCs, not only
because it is derived from parent cells, but also because it has
higher biological stability and lower immunogenicity [29].
Human amniotic epithelial cells (hAECs)
As a potential source of stem cells, hAECs are isolated from
the amniotic membrane, which is in contact with amniotic fluid
and is the layer of tissue closest to the fetus. Many studies have
reported the immunomodulatory effects of hAECs on acquired
immune cells and innate immune cells. In addition, hAECs can
differentiate into many cells of mesodermal and ectodermal
origin, including neuronal cells, pancreatic cells, hepatocytes,
adipocytes, cardiomyocytes and myocytes. Besides, hAECs are
able to inhibit the proliferation of B cells and suppress the migration and proliferation of neutrophils and macrophages [30].
Additionally, hAECs inhibited the activation of CD4+ T cells and
reduced the production of pro-inflammatory cytokines by CD4+
T cells. According to the literature, hAECs significantly enhance
proliferating cell nuclear antigen (PCNA), which is essential for
accurate DNA replication [31]. Punyadeera et al [32] analyzed
the mRNA expression levels of all known vascular endothelial
growth factor ligands and receptors in human endometrium
collected during the menstrual and proliferative phases of the
menstrual cycle. The results showed that PCNA was most abundant in both epithelial and mesenchymal tissues in the proliferative phase. However, the expression of hAECs was reduced
in the endometrium of mice during the secretory phase, suggesting that hAECs may have a role in promoting endometrial
proliferation. Vascular endothelial growth factor was mainly expressed during the proliferative and menstrual phases, which is
associated with the maintenance and formation of micro vessels and the reconstruction of endometrial tissue.
Chen et al [33] verified that intrauterine adhesion release
combined with hormone replacement therapy significantly increased endometrial vascular endothelial growth factor expression and microvascular density in patients with severe uterine
adhesions. Besides, patients with better outcome did have
more VEGF expression and denser microvasculature compared
to those with poor treatment response. hAECs were found to
increase VEGF expression in a model of intrauterine adhesions
by Zhou et al [34], suggesting that hAECs have the potential to
promote angiogenesis in the injured endometrium. The estrogen receptor, a nuclear transcription factor, binds to estrogen to
promote endometrial cell proliferation and metabolism. In one
study, umbilical cord-derived mesenchymal stromal cells were
loaded onto a collagen scaffold and transplanted into the uterine cavity after a uterine adhesion separation procedure [35].
3 months later after surgery, patients had an increase in mean
maximum endometrial thickness and a decrease in uterine adhesion scores compared to pre-treatment. Histological studies
showed upregulated levels of estrogen receptor, wave protein
and vascular hemophilia factor expression, suggesting improved
endometrial proliferation, differentiation and neovascularization after treatment. Another study came to a similar conclusion that hAECs significantly improved the uterine architecture
after uterine adhesions. hAECs treatment resulted in thickened
endometrium, increased number of endometrial glands, and
reduced fibrosis, which in turn produced more micro vessels.
Expression levels of vascular endothelial growth factor, PCNA
and estrogen receptor were increased in hAECs-treated endometrium, indicating improved angiogenesis and stromal cell
proliferation. Finally, hAECs also increased pregnancy outcome,
pregnancy rate and fetal number in mice with uterine adhesions [36].
Acupuncture and physical therapy
Acupuncture is a representative of traditional Chinese medicine and has accumulated much clinical experience in the treatment of gynecologic infertility. For thin endometrium, acupunc-
ture therapy has shown the same great potential for clinical
application. Acupuncture is an important part of traditional Chinese medicine, which applies mechanical stimulation through
the use of needles at specific acupuncture points, thereby regulating the body’s functions.
Several studies have shown that acupuncture treatment
for patients can effectively improve the clinical pregnancy rate
and increase ovarian-uterine blood perfusion at embryo implantation [37]. Performing transcutaneous acupoint electrical
stimulation during the pre-implantation phase can promote
increased expression of endometrial angiogenesis and stromal cell proliferation-related factors, resulting in a significant
improvement in endometrial tolerance [38]. Mechanistic studies have shown that progesterone levels were significantly increased after transcutaneous acupoint electrical stimulation
treatment, and integrin family proteins and leukemia inhibitory
factors were significantly increased and positively correlated
with the increase in progesterone. Li Yu et al. randomly divided
90 patients who failed to conceive due to unexplained endometrial dysplasia into two groups. The experimental group was
treated with transcutaneous electrical acupoint stimulation
from the 5th day of menstruation, supported by progesterone
after ovulation and embryo transfer three days after ovulation; the control group was given conventional estradiol valerate and
progesterone support. The results showed that the pre-transfer
thickness and endometrial type improved significantly in the experimental group compared with the control group. Among the
subendometrial blood flow parameters, the resistance index
and fluctuation index of the experimental group were significantly lower than those of the control group, and the difference
was statistically significant (P<0.05). In terms of clinical pregnancy rate, the experimental group was higher than the control
group, and the difference was statistically significant.
Zhang et al [39] evaluated the effect of transcutaneous electrical acupoint stimulation on pregnancy rates in women. This
was a prospective, randomized, single-blind placebo-controlled
clinical trial that included patients who underwent cryopreserved embryo transfer or fresh cycle in vitro fertilization with
or without intracytoplasmic single sperm injection. The results
showed that one day before transplantation, administration of
transcutaneous electrical stimulation of acupuncture points
for 30 min increased clinical pregnancy rate by 13%, and administration of 2 transcutaneous electrical stimulation of acupuncture points 1 day before transplantation and 2 times after
transplantation increased clinical pregnancy rate by 20%. Low-frequency electrical stimulation at 2 Hz was superior to high-frequency electrical stimulation at 100 Hz, and acupuncture
points on the abdominal dorsum (Gui Lai, Zi Gong, Guan Yuan,
and Shen Yu) were more beneficial than acupuncture points on
the extremities (Xue Hai, Di Ji, Zu San Li, and Tai Xi) in terms
of fertility and clinical pregnancy rate [39]. Meng Qingyu et al
[40] observed the effect of electroacupuncture combined with
bone marrow mesenchymal stem cell injection on estrogen and
progesterone receptors in thin endometrium of rats. The results
showed that the uterine coefficient and the expression of Ki67,
estrogen receptor, and progesterone receptor were significantly higher in the electroacupuncture combined with bone
marrow MSC injection group compared with the control group,
and this effect was superior to that of bone marrow MSC injection alone. Similar conclusions were reached by You et al. who
found that high-frequency electroacupuncture was effective in
improving blastocyst implantation in rats with impaired endometrial tolerance. High-frequency electroacupuncture significantly increased endometrial thickness and number of pinnae.
This effect may be achieved by enhancing the LIF/STAT3 signaling pathway in rats [41]. The above evidence demonstrates that
acupuncture therapy promotes endometrial growth, improves
endometrial tolerance, and ultimately promotes embryo implantation and clinical pregnancy.
Several physical therapies including pulsed electromagnetic
fields and massage have also had a positive impact on improving
endometrial tolerance and increasing endometrial thickness.
Merhi Z et al. combined transcutaneous ozone therapy with
pulsed electromagnetic field therapy to treat patients with thin
endometrium. The results showed that ozone with pulsed EMF
therapy had vasodilatory, anti-inflammatory and antioxidant effects and successfully improved endometrial lining thickness in
all patients, with two-thirds of patients becoming pregnant after
single embryo transfer [42]. Yang et al. investigated the effect
of pelvic floor neuromuscular electrical stimulation therapy in
improving endometrial thickness. The mean endometrial thickness before and after the treatment group was 5.60 mm and
7.93 mm, respectively, compared with 5.50 mm and 6.78 mm
in the control group, with statistically significant differences, so
neuromuscular electrical stimulation therapy may be effective
in patients with thin endometrium [43]. Electro-ultrasound is a new type of physical therapy currently available, which combines transcutaneous acupoint electrical stimulation technique,
pelvic floor neuromuscular electrical stimulation technique and
acupoint ultrasound technique. Acupuncture point ultrasound
is a new acupuncture technique that uses the technique of
ultrasound to simulate acupuncture to achieve a non-invasive
acupuncture effect. Zhang et al. [44] 2021 studied 80 patients
with thin endometrial infertility, in which 40 patients in the control group were treated with estradiol valerate and 40 patients
in the observation group were treated with estradiol valerate
in combination with electro-ultrasound. The results indicated
that the endometrial thickness, morphology and volume improved in both groups, and the difference was more obvious
in the observation group (P<0.05). After treatment, the uterine
artery resistance index (RI) and type I flow ratio were significantly reduced and type III flow ratio was significantly increased
in the observation group, and the endometrial and subendometrial vascularization index (VI), blood flow index (FI) and
vascularized flow index (VFI) were significantly improved in the
observation group, and the differences were statistically significant (P<0.001). The clinical pregnancy rate in the observation
group was higher than that in the control group, and the difference was statistically significant (P<0.01). In addition, a study
found that pelvic floor muscle massage can effectively improve
the clinical pregnancy rate. The mechanism is to induce muscle contraction, increase intra-abdominal pressure, accelerate
pelvic blood flow, reduce uterine artery blood flow resistance,
and increase subendometrial blood flow and perfusion, which
improves the thickness and structure of the endometrium and
improves the active function and hormone levels of the uterus
and ovaries [45].
Conclusion
As a global disease, infertility affects a large number of
women and is both a social and a medical problem. Given the
important role of the endometrium in maternal health and reproduction, it is crucial to maintain its physiological structure,
eliminate its defects and promptly recover after damage. Several treatments have been developed, such as granulocyte
colony-stimulating factor, sildenafil, low-dose aspirin, stem
cell therapy, acupuncture and physical therapy, among others.
Overall, some of the newer therapies, including granulocyte colony-stimulating factor and stem cell therapy, may enjoy many
advantages over conventional therapies. However, there is still
room for improvement in these therapies and much research is
needed to maximize the potential of emerging new therapies.
Finally, as the feasibility of acupuncture and physical therapy for thin endometrium is proven, these therapies should likewise
receive adequate attention.
Declarations
Authors' contributions: XT and KN wrote this manuscript;
XT prepared all the figures improved the language of the manuscript; KN conceived the structure and revised the manuscript;
all authors read and approved the final manuscript.
Competing interests: The authors declare that they have no
competing interests.
Declarations: All authors declare they have no actual or potential competing interests.
Ethics approval and consent to participate: Not applicable.
Consent for publication: All authors have given their consent for publication.
Availability of data and materials: The data explored during
the current study was available from the corresponding author
on reasonable request.
Funding: Not applicable.
Acknowledgements: Not applicable.
Consent for publication section: Not applicable.
References
- Simón C, Moreno C, Remohí J, Pellicer A. Molecular interactions
between embryo and uterus in the adhesion phase of human
implantation. Human reproduction (Oxford, England). 1998;13:
219-232.
- Simón C, Landeras J, Zuzuarregui JL, Martín JC, Remohí J, et al.
Early pregnancy losses in in vitro fertilization and oocyte donation. Fertility and sterility. 1999; 72: 1061-1065.
- Pellicer A, Rubio C, Vidal F, Mínguez Y, Giménez C, et al. In vitro
fertilization plus preimplantation genetic diagnosis in patients
with recurrent miscarriage: an analysis of chromosome abnormalities in human preimplantation embryos. Fertility and sterility. 1999; 71: 1033-1039.
- Adamson GD, de Mouzon J, Chambers GM, Zegers-Hochschild
F, Mansour R, et al. International Committee for Monitoring Assisted Reproductive Technology: world report on assisted reproductive technology, 2011. Fertility and sterility. 2018; 110:1067-1080.
- Hou X, Liu Y, Streuli I, Dällenbach P, Dubuisson J, et al. Endometrial Regeneration in Asherman’s Syndrome: Clinical and
Translational evidence of Stem Cell Therapies. Current stem cell
research & therapy. 2019; 14: 454-459.
- Bashiri A, Halper KI, Orvieto R. Recurrent Implantation Failure-update overview on etiology, diagnosis, treatment and future
directions. Reproductive biology and endocrinology : RB&E. 2018; 16: 121.
- Jensen JR, Witz CA, Schenken RS, Tekmal RR. A potential role for
colony-stimulating factor 1 in the genesis of the early endometriotic lesion. Fertility and sterility. 2010; 93: 251-256.
- Gleicher N, Vidali A, Barad DH. Successful treatment of unresponsive thin endometrium. Fertility and sterility. 2011; 95:
2123.e2113-2127.
- Gleicher N, Kim A, Michaeli T, Lee HJ, Shohat-Tal A, et al. A pilot cohort study of granulocyte colony-stimulating factor in the
treatment of unresponsive thin endometrium resistant to standard therapies. Human reproduction (Oxford, England). 2013;
28: 172-177.
- Lucena E, Moreno-Ortiz H. Granulocyte colony-stimulating factor (G-CSF): a mediator in endometrial receptivity for a patient
with polycystic ovary (PCO) undergoing in vitro maturation
(IVM). BMJ case reports. 2013; 2013.
- Li Y, Pan P, Chen X, Li L, Li Y, et al. Granulocyte colony-stimulating
factor administration for infertile women with thin endometrium in frozen embryo transfer program. Reproductive sciences
(Thousand Oaks, Calif). 2014; 21: 381-385.
- Kunicki M, Łukaszuk K, Woclawek-Potocka I, Liss J, Kulwikowska
P, et al. Evaluation of granulocyte colony-stimulating factor effects on treatment-resistant thin endometrium in women undergoing in vitro fertilization. BioMed research international.
2014; 2014: 913235.
- Eftekhar M, Sayadi M, Arabjahvani F. Transvaginal perfusion of
G-CSF for infertile women with thin endometrium in frozen ET
program: A non-randomized clinical trial. Iranian journal of reproductive medicine. 2014; 12: 661-666.
- Tehraninejad E, Davari Tanha F, Asadi E, Kamali K, et al. G-CSF
Intrauterine for Thin Endometrium, and Pregnancy Outcome.
Journal of family & reproductive health. 2015; 9: 107-112.
- Barad DH, Yu Y, Kushnir VA, Shohat-Tal A, Lazzaroni E, et al. A
randomized clinical trial of endometrial perfusion with granulocyte colony-stimulating factor in in vitro fertilization cycles:
impact on endometrial thickness and clinical pregnancy rates.
Fertility and sterility. 2014; 101: 710-715.
- Miralaei S, Ashrafi M, Arabipoor A, Zolfaghari Z, Taghvaei S. The
incidence rate of unresponsive thin endometrium in frozen embryo transfer cycles: A case-series of therapy with granulocyte
colony stimulating factor. International journal of reproductive
biomedicine. 2019; 17: 923-928.
- Lee D, Jo JD, Kim SK, Jee BC, Kim SH. The efficacy of intrauterine
instillation of granulocyte colony-stimulating factor in infertile
women with a thin endometrium: A pilot study. Clinical and experimental reproductive medicine. 2016; 43: 240-246.
- Aghebati-Maleki L, Dolati S, Zandi R, Fotouhi A, Ahmadi M, et al.
Prospect of mesenchymal stem cells in therapy of osteoporosis:
A review. Journal of cellular physiology. 2019; 234: 8570-8578.
- Li L, Xie T. Stem cell niche: structure and function. Annual review
of cell and developmental biology. 2005; 21: 605-631.
- Zakrzewski W, Dobrzyński M, Szymonowicz M, Rybak Z. Stem
cells: past, present, and future. Stem cell research & therapy.
2019; 10: 68.
- Nouri N, Aghebati-Maleki L, Yousefi M. Adipose-Derived Mesenchymal Stem Cells: A Promising Tool in the Treatment of pre mature ovarian failure. Journal of reproductive immunology. 2021;
147: 103363.
- Caplan AI. All MSCs are pericytes? Cell stem cell. 2008; 3: 229-230.
- Mikos AG, Herring SW, Ochareon P, Elisseeff J, Lu HH, et al. Engineering complex tissues. Tissue engineering. 2006; 12: 3307-3339.
- Schwartz RE, Reyes M, Koodie L, Jiang Y, Blackstad M, et al. Multipotent adult progenitor cells from bone marrow differentiate
into functional hepatocyte-like cells. The Journal of clinical investigation. 2002; 109: 1291-1302.
- Dai W, Hale SL, Martin BJ, Kuang JQ, Dow JS, et al. Allogeneic mesenchymal stem cell transplantation in postinfarcted rat
myocardium: short- and long-term effects. Circulation. 2005;
112: 214-223.
- Zhao J, Zhang Q, Wang Y, Li Y. Uterine infusion with bone marrow mesenchymal stem cells improves endometrium thickness
in a rat model of thin endometrium. Reproductive sciences
(Thousand Oaks, Calif). 2015; 22: 181-188.
- Jing Z, Qiong Z, Yonggang W, Yanping L. Rat bone marrow mesenchymal stem cells improve regeneration of thin endometrium
in rat. Fertility and sterility. 2014; 101: 587-594.
- Saribas GS, Ozogul C, Tiryaki M, Alpaslan Pinarli F, Hamdemir Kilic S. Effects of uterus derived mesenchymal stem cells and their
exosomes on asherman’s syndrome. Acta histochemica. 2020;
122: 151465.
- Liao Z, Liu C, Wang L, Sui C, Zhang H. Therapeutic Role of Mesenchymal Stem Cell-Derived Extracellular Vesicles in Female
Reproductive Diseases. Frontiers in endocrinology. 2021; 12:
665645.
- Gan L, Duan H, Xu Q, Tang YQ, Li JJ, et al. Human amniotic mesenchymal stromal cell transplantation improves endometrial
regeneration in rodent models of intrauterine adhesions. Cytotherapy. 2017; 19: 603-616.
- Moldovan GL, Pfander B, Jentsch S. PCNA, the maestro of the
replication fork. Cell. 2007; 129: 665-679.
- Punyadeera C, Thijssen VL, Tchaikovski S, Kamps R, Delvoux B,
et al. Expression and regulation of vascular endothelial growth
factor ligands and receptors during menstruation and post-menstrual repair of human endometrium. Molecular human reproduction. 2006; 12: 367-375.
- Chen Y, Chang Y, Yao S. Role of angiogenesis in endometrial repair of patients with severe intrauterine adhesion. International
journal of clinical and experimental pathology. 2013; 6: 1343-1350.
- Zhou Q, Wu X, Hu J, Yuan R. Abnormal expression of fibrosis
markers, estrogen receptor α and stromal derived factor-1/chemokine (C-X-C motif) receptor-4 axis in intrauterine adhesions.
International journal of molecular medicine. 2018; 42: 81-90.
- Cao Y, Sun H, Zhu H, Zhu X, Tang X, et al. Allogeneic cell therapy
using umbilical cord MSCs on collagen scaffolds for patients with
recurrent uterine adhesion: a phase I clinical trial. Stem cell research & therapy. 2018; 9: 192.
- Li B, Zhang Q, Sun J, Lai D. Human amniotic epithelial cells improve fertility in an intrauterine adhesion mouse model. Stem
cell research & therapy. 2019; 10: 257.
- Zhang Mingmin, Huang Guangying, Lu Fuer. Effect of acupuncture on the pregnancy rate in embryo transfer and mechanisms:
A randomized and control study. Chinese acupuncture. 2003; 7-9.
- Feng XJ. The influence of transcutaneous acupoint electrical
stimulation(TENS) with HAN’S acupoint nerve stimulator (HANS)
on reproductive outcome in patients treated with in-vitro-fertilization(IVF)/intracytoplasmic sperm injection (ICSI)and the
preliminary mechanism research. MA thesis. Shandong Chinese
medical school. 2011.
- Zhang R, Feng XJ, Guan Q, Cui W, Zheng Y, et al. Increase of success rate for women undergoing embryo transfer by transcutaneous electrical acupoint stimulation: a prospective randomized
placebo-controlled study. Fertility and sterility. 2011; 96: 912-916.
- Meng Qing-Yu,Xi Jin,Xia Liang-Jun. Effect of combined administration of electroacupuncture and mesenchymal stem cells on
expression of endometrium estrogen receptor and progesterone receptor in thin endometrium rat. Acupuncture research.
2021; 46 : 385-390.
- You F, Du X, Zhang T, Wang Y, Lv Y, et al. High-frequency electroacupuncture improves endometrial receptivity via regulating
cell adhesion molecules and leukemia inhibitory factor / signal
transducer and activator of transcription signaling pathway. Bioengineered. 2021; 12: 10470-10479.
- Merhi Z, Moseley-LaRue R, Moseley AR, Smith AH, Zhang J.
Ozone and pulsed electro-magnetic field therapies improve
endometrial lining thickness in frozen embryo transfer cycles:
Three case reports. Medicine. 2019; 98: e16865.
- Bodombossou-Djobo MM, Zheng C, Chen S, Yang D. Neuromuscular electrical stimulation and biofeedback therapy may improve endometrial growth for patients with thin endometrium
during frozen-thawed embryo transfer: a preliminary report.
Reproductive biology and endocrinology : RB&E. 2011; 9: 122.
- He Ying, Zhang Qing, Liu Pan. Clinical efficacy of bioelectrical
stimulation combined with ultrasound “acupuncture” in the
treatment of patients with thin endometrial infertility. Chinese
Journal of Practical Gynecology and Obstetrics, 2021; 37: 1254-1258.
- Shen L. Effects of Pelvic Floor Muscle Massage on the Pregnancy
Outcome of Frozen Embryo Transfer in Patients with Thin Endometrium. Computational and mathematical methods in medicine. 2022; 2022: 2803363.