Introduction
The characteristics of the aging process are biochemical,
morphological, physiological and psychological alterations,
which predispose individuals to the progressive loss of the ability to adapt to the environment, to the appearance and worsening of diseases, altering their motor and cognitive abilities [1].
Physiological alterations with impact on mobility, balance, and
physical performance stand out, making the individual more
susceptible to falls and the fear of falling, which can cause possible fractures and consequent immobility [2-5].
Physiological alterations caused by aging can be mitigated
with the practice of physical exercises, since their benefits
promote greater autonomy and quality of life in the elderly
population [3,6,7]. Studies have evidenced that certain types
of exercises, such as walking, balance, coordination, functional
training, strengthening exercises, and other three-dimensional
training programs are effective for improving balance in the
elderly [8] muscle strength, mobility, and functional independence [9,10].
The conventional proprioceptive training promotes positive
effects on functionality and, consequently, reduction of falls in
the elderly [11-13]. Recently, the emergence of new technologies such as virtual reality, also known as "exergames", has
been used in clinical practice with therapeutic purposes such
as gait [14], balance [14,15], muscle strength [14,16], and falls
[17,18].
Although conventional and virtual proprioceptive training
are alternatives to reduce losses due to aging, there is no consensus in the scientific literature as to which modality provides
better performance in functionality and consequently reduction of the fear of falling in elderly women. Therefore, this study
aimed to evaluate and compare the effects of conventional proprioceptive training and virtual reality on the functionality and
fear of falling of elderly women.
Methods
Study Design and Setting
This study was developed according to the recommendations of CONSORT (Consolidated Standards of Reporting Trials)
[19]. It consists of a randomized controlled clinical trial, the
sample was composed of elderly women participating in four
Senior Citizenship Groups, located in the city of Jequié, Bahia,
Brazil.
The choice for female participants was due to the observation during the visits to the groups that only two elderly men
were attending the groups, thus making it impossible for them
to participate, since this would compromise the homogeneity
of the characteristics between the groups.
Sample
Participants
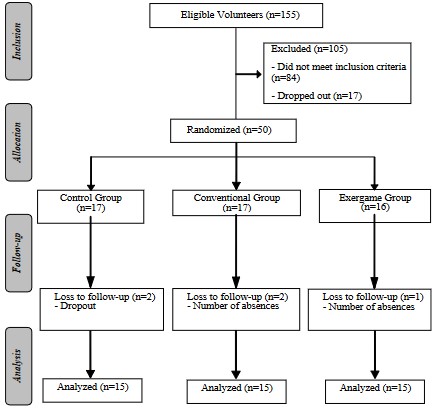
The sample size was defined based on the results of a pilot
study with 5 elderly women in each group and considering as
outcome the difference (i.e., performance before training or
control - performance after training or control) in the Time Up
Go Test (TUGT) (described ahead). For the sample size calculation, we considered α=0.05 and the power of the test (1-β) =
0.95, with 3 groups (control x conventional x exergame), which
obtained a sample number of 36 individuals (i.e., 12 in each
group). Considering the possibility of sample loss throughout
the 8-week intervention, the sample size was estimated with
a loss margin of 25% in each group, and therefore a sample
number of 15 elderly women per group was expected (i.e., total
sample size of 45 elderly women) (Figure 1). The sample size
calculation was performed in the G*Power® version 3.1 software.
As inclusion criteria, it was established that the elderly women should present: a) minimum age of 60 years and maximum
of 79 years; b) had not been practicing any type of physical exercise (oriented and regular) in the last three months or had
been practicing physical exercises, but not enough to be classified as active due to non-compliance with the recommendations regarding duration, i.e., less than 150 minutes per week
[20]; c) absence of cognitive deficit assessed through the MiniMental State Examination (MMSE) [21], the version adapted
for the Brazilian population. The absence of cognitive disorder
followed the cut-off values according to education: Illiterate ≥ 13 points, 1 to 8 incomplete years ≥ 18 points, and 8 years or
more of schooling ≥ 26 points [22]; d) absence of diagnosis of
diabetes mellitus; e) absence of vestibulopathies; f) absence of
cardiovascular diseases limiting exercise; g) absence of any visual or auditory difficulty that would compromise the proposed
training sessions; h) absence of skin lesions on the feet and amputations; i) absence of osteoarticular lesions that could hinder
or make it difficult to carry out the training sessions; j) independent deambulation and locomotion without auxiliary devices;
k) absence of claudication or any other alteration in the gait pattern for any reason; l) availability to attend the training sessions
held throughout the study.
The following were excluded from the study: a) elderly women who had attended another proprioceptive rehabilitation
program during the training or within the last three months;
b) those who had participated in less than 75% of the training
program.
Before the interventions, a pilot study was conducted with
15 elderly women, which allowed adjustments in the participants' training time, better handling of the resources used, and
standardization of some evaluation methods. After screening
the participants according to the established criteria, 50 elderly
women remained in the sample, which were submitted to stratified randomization by age (60-69/70-79) and BMI (low/high).
From the stratification, the participants were distributed into
four groups: age (60-69) and low BMI, age (60-69) and high BMI,
age (70-79) and low BMI, and age (70-79) and high BMI.
Subsequently, a code was created for each participant and
randomization was performed in blocks of three individuals for
each stratum. The blocks were randomized using Microsoft® Excel version 2013, and then the codes were distributed in three
arms of the study (conventional group, exergame group, and
control group). A researcher with no clinical involvement in the
trial, thus ensuring the confidentiality of the allocation, performed the entire process.
Intervention protocol
The control and conventional groups were composed of 17
participants and the exergame group was composed of 16 participants, and at the end of the study each group ended with
15 participants. The losses were related to participation below
75% of the training program (three elderly women) and dropouts (two elderly women), totaling five losses (Figure 1).
In the present study, the blinding of the participants and
the researchers was not possible, since both were present and
experienced the execution of the proposed training sessions.
However, blinding was possible for the evaluators, who did not
know to which group each elderly woman was allocated. The
researchers consisted of previously trained physical therapy
students and physical therapists.
The control group (GCT), during the intervention period, did
not participate in any training modality; the conventional group
(GCV) participated in conventional proprioceptive training; and
the exergame group (GEX) participated in proprioceptive training based on virtual realities.
The training was performed three times a week, during
8 weeks, for 24 sessions, duration of 50 minutes per session,
with a minimum interval of 48 hours between each session. The
training protocol was organized as follows: warm-up (10 min),
proprioceptive training (30 min), and cool-down (10 min), with monitoring of blood pressure and heart rate before and after
the activities.
Before the first session, the objectives of the activities were
presented to the participants and, for the familiarization they
were allowed to make one attempt per activity on the same
day as the first session. During the first two sessions the elderly
women were assisted verbally and manual contact from the researchers, helping them in the best and most correct way to
move in order to reach the training objectives and promote postural correction.
The warm-up consisted of a walk (4 minutes) and stretching exercises for the muscles of the upper and lower limbs,
and spine (6 minutes). The cooling down was performed with
breathing exercises (5 minutes), and stretching exercises (5
minutes). The participants were warned not to alter their activities of daily living during the intervention period, thus avoiding
possible influences of external factors on the outcomes of the
research.
The training sessions were suspended in case the participants presented vertigo, malaise, muscle pain, increased blood
pressure, or any other physical discomfort. At the end of the
study, for ethical reasons, the CGT received conventional proprioceptive training under the same conditions as those established in the VGC protocol.
The conventional proprioceptive training protocol involved
gait, balance, and proprioception training, and was spatially organized in the form of a circuit with different textures and obstacles, consisting of seven stations. The materials used were:
1 mattress of dimension 120 X 70 X 10 cm (station 1), 1 foam
module - mini beam of dimension 190 X 22 X 10 cm (station 2),
4 agility rings with 42 cm diameter (station 3), 1 proprioceptive
lateral board of dimension 60 X 36 X 8 cm (station 4), 2 agility
cones of the dimensions 23 X 14 cm (station 5), 1 proprioceptive
disc with a diameter of 40 cm (station 6), and 3 agility barriers of
the dimensions 70 X 15/ 70 X 20/ 70 X 25 cm (station 7).
The elderly women participated, in groups of two or three,
in specific exercises at each station that combined sensory and
motor stimulation, as follows:
- Station 1: Lateral strides (right and left), forward and backward strides on unstable surface (dense mattress), exercises in
bipodal and unipodal support (right and left) with eyes open
and closed, agility training with ball throwing.
- Station 2: Forward, backward and sideward march (right
and left) with narrow base on unstable surface (foam mini
beam), march alternating between floor and mini beam, agility
training with ball throw.
- Station 3: Forward, backward, sideways and cross-legged
march between the agility rings.
- Station 4: Side-to-side and front-to-back exercise on the
proprioceptive lateral board with eyes open and closed, agility
training with ball throw.
- Station 5: Forward, backward and sideward march between
cones with narrowed base and circumferential path with full
foot support, with heel support only, and with forefoot support
only.
- Station 6: Exercises on proprioceptive disk with multidirectional shifts with eyes open and closed, agility training with ball throw.
- Station 7: Forward, backward and sideward march over
agility barriers, agility training with ball throw.
The participants remained at each station for two minutes, with a thirty-second break between stations. After going
through the seven stations, the course was repeated on the
front, side, and back through all the stations continuously without breaks, with only a thirty-second break at the end of each
circuit, until the proposed time of 30 minutes was completed.
The degree of difficulty was increased throughout the training via the speed of execution of the activities. In all the sessions, a researcher assisted each elderly woman on the execution and physical capacity of each participant was taken into
consideration in relation to the execution of the activities. The
exercises in the conventional training protocol were based on
the literature [23-25].
The proprioceptive training based on virtual realities "exergames" was performed using the Xbox Kinect One videogame
from Microsoft®®. This console uses motion sensor technology,
the Kinect, which captures the movements of the players, they
are sensitive to changes in direction, speed, and acceleration,
thus allowing games to be controlled with body movement,
without the need for any manual control [26].
The game used was Kinect Sports Rivals, which simulates six
sports activities: jet ski racing, climbing, soccer, bowling, tennis
and target shooting. The selection was guided by the analysis of
the motor demands offered by the games. The exercises ranged
from basic motor skills: squatting and lifting, jumping, turning,
lumbar flexion, side-to-side and anterior-posterior displacement, and moving the arms in all directions, to more complex
motor skills that stimulated coordination, balance, stability, and
proprioception.
The more complex exercises consisted in extending an arm
and flexing the contralateral leg associated with body thrust
(climbing game); performing side-to-side displacement associated with flexion/extension and adduction/abduction movements of the upper limbs (tennis game); perform kicks, displacements, and body rotation (soccer game); perform hip and
knee flexion, with trunk rotation and inclination (jet ski game);
perform hip, knee, and ankle flexion with lower limbs in alternate position, associated with trunk inclination and shoulder
flexion/extension movement (bowling game).
The selection process of the games was carried out during
the pilot study, and in the main study only the games that were
not difficult to play, that worked motor skills, and were more
accepted by the elderly women were used. Thus, the game "target shooting" was excluded because it was repetitive, did not
work motor skills in a satisfactory way, and presented a degree
of difficulty that did not evolve gradually, which meant that it
was not well accepted by the elderly women in the pilot study.
The training with exergames was carried out in a room with
no objects that could interfere with the performance of the elderly women, in which the games were projected on the wall
using an Epson PowerLite S8+ projector and a set of Multilaser© 60 WRms Sp088 speakers. The participants were accompanied by researchers, performed the activities in pairs, barefoot, and positioned in front of the Kinect sensor at a distance
of three meters.
Three games were used per session and the duration of each game was 10 minutes, for a total of 30 minutes. The order of the
games in each session was randomized, one game was replaced
by another every six training sessions by random selection, allowing the participants to have contact at the end of the training with all five selected games.
Outcome assessment
For the evaluation of the study outcomes, a questionnaire
composed of sociodemographic information, related to health,
functionality, and fear of falling was used. The sociodemographic variables used were: age (complete years), marital status
(with partner, without partner), education (illiterate, elementary, middle, higher education) and monthly family income in
Brazillian Reais (BRL). For the categorization of family income
the median was used, establishing the following categories
(≤954.00 BRL, >954.00 BRL). The health-related variables were:
Body Mass Index (BMI), presence of diagnosed diseases (yes,
no), musculoskeletal pain in the last 7 days (yes, no), musculoskeletal pain in the last 12 months (yes, no), and medications
(yes, no).
The functionality evaluation was composed of balance, functional mobility and functional physical performance of the lower limbs. For balance the Berg Balance Scale (BBS) translated
and validated for the Brazilian population was used, which consists of functional clinical tests that evaluate the static and dynamic balance of individuals in daily activities. The BBS consists
of 14 tasks, grouped into: transfers (tasks 1, 4 and 5), stationary
trials (tasks 2, 3, 6 and 7), functional reach (task 8), rotational
components (tasks 9, 10 and 11), and decreased base of support (task 12, 13 and 14). The scores used in each task were 0
for inability to perform activities up to 4 points for performing
tasks independently, and the total scores ranged from 0 to 56
points, in which the maximum score corresponds to the best
performance [27].
To assess functional mobility, the Time Up and Go Test
(TUGT) was used, proposed [28], measured in seconds, evaluating the time spent by the participants to get up from a chair (45
cm high), walk a distance of three meters, turn around, walk
towards the chair and sit down again. The TUGT is a sensitive
and specific measure to identify elderly at risk of falling and is
widely used to assess the functional mobility of this population.
Independent individuals without balance alterations perform
the test in ≤10 seconds (low fall risk); those who are dependent
in basic transfers spend ≤20 seconds (medium fall risk). Individuals who need more than 20 seconds to perform the test are
dependent in many activities of daily living and mobility (high
risk of falls) [28].
To evaluate the functional physical performance of the lower
limbs, we used the Short Physical Performance Battery (SPPB),
which consists of a battery of tests proposed by Guralnik in
1994, and adapted and validated for the Brazilian population
[29]. This instrument evaluates physical capacity, prioritizing
tests of lower limb function, and is composed of three steps:
balance, gait speed, and getting up and sitting down from a
chair. For the balance test, the participants were instructed to
maintain themselves in the bipedal posture in the following positions: feet together (side-by-side); one foot partially in front
of the other (semi-tandem stand); and one foot in front of the
other (tandem stand), maintaining themselves for 10 seconds in
each position. For the walking speed test, a distance of 3 meters
was adopted, and the participants were instructed to walk this
distance at their usual pace, with two times recorded (round trip), and the shortest execution time was considered. The chair
standing and sitting test was performed using a 44 cm chair, in
which the participants stood up and sat down in the chair five
consecutive times, without the aid of their upper limbs, and as
fast as possible [29].
This instrument evaluates physical capacity, prioritizing tests
of lower limb function, and is composed of three steps: balance,
gait speed, and getting up and sitting down from a chair. For the
balance test, the participants were instructed to maintain themselves in the bipedal posture in the following positions: feet
together (side-by-side); one foot partially in front of the other
(semi-tandem stand); and one foot in front of the other (tandem
stand), maintaining themselves for 10 seconds in each position.
For the walking speed test, a distance of 3 meters was adopted,
the participants were instructed to walk this distance at their
usual pace, with two times recorded (round trip), and the shortest execution time was considered. The chair standing and sitting test was performed using a 44 cm chair, in which the participants stood up and sat down in the chair five consecutive times,
without the aid of their upper limbs, and as fast as possible [29].
The three steps are scored from 0 to 4, according to the time
for each task. The total SPPB score was obtained by the sum
of the scores in the balance tests, gait speed, and getting up
from a chair five consecutive times, ranging from 0 (worst performance) to 12 points (best performance) [29].
The fear of falling was assessed by means of the Falls Efficacy
Scale - International - Brazil (FES-I-BRAZIL), a version adapted
and validated for the Brazilian population [30]. The FES-I-BRAZIL
assesses the fear of falling in 16 activities of daily living (basic
and instrumental) and socialization. The assessed items involve
from tasks of low physical demand to tasks related to postural
control, such as: cleaning the house, dressing and undressing,
preparing meals, bathing, shopping, going up and down stairs
and slopes, walking on slippery and uneven surfaces, visiting a
friend or going to a social activity. Each question is scored on a
scale of 1 to 4 points, with total values ranging from 16 points
for individuals with no concern about falling to 64 points for
individuals with extreme concern [30].
The evaluations were made in two moments: before training (T0) and after training (T1), by researchers who did not participate in the allocation process of the elderly women and had
no contact with the treatment groups. For the CGT, the participants were evaluated and reassessed following the same period
and place established for the intervention groups.
Data analysis
In the data analysis, absolute and relative frequencies were
used for categorical data, and for quantitative data mean and
standard deviation or median and interquartile range. To evaluate the homogeneous behavior of the quantitative variables
(age and BMI) at baseline in the three groups (control, conventional, and exergame) the analysis of variance (ANOVA) and
Kruskal-wallis tests were used, after checking the normality of
the data using the Shapiro-Wilk test. Pearson's chi-square test
and Fischer's exact test were used to compare the categorical
variables (marital status, education, family income, presence of
illness, pain in the past 7 days and 12 months, and medications)
between groups at the beginning of the study.
In the inferential analysis (parametric or non-parametric)
for the intragroup comparisons of baropodometric variables
between two paired samples were performed using paired Student's t test or Wilcoxon test. Intergroup comparisons between
three independent samples were performed by means of oneway analysis of variance (ANOVA) tests, and in case of statistical difference, Tukey's post-hoc test was used; or Kruskal-wallis,
and in case of statistical difference, Dunn's post-hoc test was
used.
In the case where the dependent variable (SPPB) showed a
significant difference at baseline we conducted the analysis of
covariance (ANCOVA), using the initial measurements of these
variables (T0) as a covariate to control the effect of these variables on the difference in means (T1-T0) between the groups.
After analysis, Sidak's post-hoc test was used.
The calculation of the effect size was performed for the comparisons between groups (i.e., comparisons of the differences
between T0 and T1), and the partial eta2 parameter (partia leta
squared, η2 partial) was adopted as an indicator of effect size, as
recommended by Lakens [31] and Murphy et al. [32]. The interpretation of effect size followed the recommendations of Cohen
[33], who suggests a small effect size when η2 = 0.01, medium
when η2 = 0.06, and large when η2 = 0.14.
The significance level adopted in all analyses was 5% (α =
0.05), and the data were analyzed using IBM Statistical Package
for the Social Sciences (SPSS) for Windows, version 21.0.
Ethics and registration
This study was conducted in accordance with resolution no.
466/2012 of the National Health Council and approved by the
Research Ethics Committee of the Universidade Estadual do
Sudoeste da Bahia (Southwestern Bahia State University), under protocol no. 2.627.047, CAAE: 46887315.1.0000.0055. The
study was registered in the Brazilian Registry of Clinical Trials
(REBEC) database, registration number RBR-592yyp.
Results
Among the 50 elderly women who started participating in
the research (17 control, 17 conventional, and 16 exergame),
only 5 did not complete the study. Adherence to the intervention programs was 88.2% for the control and conventional
groups, and 94.1% for the exergame group.
Regarding sociodemographic characteristics, it was observed
that the mean age of the participants was 69.1 ± 6.0 years;
77.8% lived without a partner; 71.1% were illiterate or had elementary school education, 22.2% had high school education,
and 6.7% had higher education. The majority (68.9%) declared
a monthly family income ≤954.00 BRL.
According to the health-related variables, the average BMI
was 26.6 ± 4.4 Kg/m2; 82.2% reported the presence of diseases;
77.8% and 84.4% had musculoskeletal pain in the last 7 days
and the last 12 months, respectively; and 95.6% used medications.
There were no statistically significant differences between
the groups at baseline (control, conventional and exergame)
regarding the distribution between: median age (p= 0.451,
Kruskal-Wallis test); mean BMI (p=0.840, one-way ANOVA);
marital status (p=0.550, chi-square test); education (p=0, 800,
chi-square test); family income (p= 0.779, chi-square test); presence of diseases (p=1.000, chi-square test); musculoskeletal
pain (p=0.280, chi-square test); use of medications (p=1.000,
chi-square test), thus demonstrating homogeneity in the allocation of participants between the groups.
The analysis of mobility, balance, lower limb performance,
and fear of falling in the control, conventional, and exergame
groups at T0 showed that with the exception of SPPB, the variables showed no significant differences between the groups,
indicating that the three groups had similar characteristics at
study baseline (Table 1).
Table 1: Intergroup comparisons of functional mobility, bal-
ance, lower limb performance and initial fear of falling (T0) of the
elderly women participating in the study.
| Variable |
Control |
Conventional |
Exergame |
p-value |
| TUGT# |
10.19 (3.16) |
11.48 (2.75) |
11.78 (2.71) |
0.287 |
| EEB* |
55.00 (6.00) |
54.00 (4.00) |
55.00 (2.00) |
0.384 |
| SPPB# |
11.47 (0.91) |
10.13 (1.36) |
10.33 (1.99) |
0.008 |
| FES-I-Brasil* |
26.10 (17.00) |
30.00 (12.00) |
27.00 (13.00) |
0.936 |
TUGT = Time Up and Go Test; BBS = Berg Balance Scale; SPPB = Short
Physical Performance Battery; FES-I-Brazil = Falls Efficacy Scale International adapted to Brazil; # Mean (standard deviation), one-way ANOVA;
* Median (interquartile range), Kruskall-Wallis test.
The comparisons between T0 and T1 in the control group
showed a significant difference for the TUGT, indicating that,
at the end of the period evaluated, the elderly women in this
group presented significantly higher values in this variable,
which characterized a worse performance in functional mobility (Table 2).
Table 2: Intragroup comparisons (T0 vs. T1) of functional mobility, balance, lower limb performance, and fear of falling for the
control group of the elderly women participating in study.
| Variable |
T0 (baseline) |
T1 (post-treatment) |
p-value |
| TUGT# |
10.19 (3.16) |
11.36 (2.48) |
0.021 |
| EEB* |
53.27 (3.41) |
53.47 (2.80) |
0.647 |
| SPPB# |
12.00 (1.00) |
11.00 (2.00) |
0.107 |
| FES-I-Brasil* |
26.10 (17.00) |
32.00 (15.00) |
0.072 |
TUGT = Time Up and Go Test; BBS = Berg Balance Scale; SPPB = Short
Physical Performance Battery; FES-I-Brazil = Falls Efficacy Scale International adapted to Brazil; # Mean (standard deviation), Student's t test
for paired samples; * Median (interquartile range), Wilcoxon test.
The comparisons between T0 and T1 in the conventional
group showed a significant difference in all variables, indicating that, at the end of the treatment, the elderly women in this
group presented significantly better values, which characterized
an improvement in mobility, balance, lower limb performance,
and less concern about the fear of falling (Table 3).
Table 3: Intragroup comparisons (T0 vs. T1) of functional mobility, balance, lower limb performance, and fear of falling for the
conventional group of elderly women participating in study.
| Variable |
T0 (baseline) |
T1 (post-treatment) |
p-value |
| TUGT# |
11.43 (2.71) |
10.00 (3.06) |
0.001 |
| EEB* |
54.00 (4.00) |
56.00 (1.00) |
0.001 |
| SPPB# |
10.13 (1.36) |
11.40 (0.74) |
<0.001 |
| FES-I-Brasil* |
28.53 (7.53) |
24.73 (6.42) |
0.001 |
TUGT = Time Up and Go Test; BBS = Berg Balance Scale; SPPB = Short
Physical Performance Battery; FES-I-Brazil = Falls Efficacy Scale International adapted to Brazil; # Mean (standard deviation), Student's t test
for paired samples; * Median (interquartile range), Wilcoxon test.
The comparisons between T0 and T1 in the exergame group
showed a difference for BBS, SPPB, and FES-I-Brazil, indicating
that, at the end of the treatment, the elderly women in this
group presented significantly better values for these variables,
which characterized an improvement in balance, lower limb
performance, and less concern about the fear of falling (Table
4).
Table 4: Intragroup comparisons (T0 vs. T1) of functional mobility, balance, lower limb performance, and fear of falling for the
exergame group of the elderly women participating in the study.
| Variable |
T0 (baseline) |
T1 (post-treatment) |
p-value |
| TUGT# |
11.78 (2.71) |
11.02 (1.84) |
0.220 |
| EEB* |
55.00 (2.00) |
56.00 (1.00) |
0.011 |
| SPPB# |
11.00 (2.00) |
12.00 (0.00) |
0.003 |
| FES-I-Brasil* |
27.00 (13.00) |
22.00 (10.00) |
0.003 |
TUGT = Time Up and Go Test; BBS = Berg Balance Scale; SPPB = Short
Physical Performance Battery; FES-I-Brazil = Falls Efficacy Scale International adapted to Brazil; # Mean (standard deviation), Student’s t test
for paired samples; * Median (interquartile range), Wilcoxon test.
The comparative analysis of changes in mobility, balance,
lower limb performance, and fear of falling showed significant
differences between the groups. For the TUGT, SPPB, and FES-I-Brazil variables there was a better effect of conventional training and exergame when compared to the control group; while
for the BBS variable, there was a better effect of conventional
training compared to the control group.
Among all the variables studied, no significant differences
were observed between the conventional and exergame groups,
indicating a similar effect of the two trainings. Regarding the effect size, the results indicate an effect classified as large for all
variables studied (0.185 - 0.348) (Table 5).
Table 5: Intergroup comparisons of changes (T1-T0) and effect
size of functional mobility, balance, lower limb performance, and
fear of falling of the elderly female study participants. Jequié,
Bahia, 2019.
| Variable |
Control |
Conventional |
Exergame |
p-value |
η2 partial |
| TUGT# |
1.17 (1.74)a |
-1.37 (1.20)b |
-0.75 (2.27)b |
0.001 |
0.281 |
| SPPB+ |
-0.03 (1.44)a |
0.91 (1.39)b |
1.18 (1.37)b |
0.001 |
0.348 |
| EEB* |
0.00 (2.00)a |
1.00 (3.00)b |
1.00 (2.00)ab |
0.009 |
0.185 |
| FES-I-Brasil* |
0.90 (2.00)a |
-3.00 (5.00)b |
-2.00 (6.00)b |
<0.001 |
0.334 |
TUGT = Time Up and Go Test; BBS = Berg Balance Scale; SPPB = Short
Physical Performance Battery; FES-I-Brazil = Falls Efficacy Scale International adapted to Brazil; # Difference of means T1-T0 (standard deviation), one-way ANOVA, Tukey post-hoc; + Difference of means T1-T0
(standard deviation), ANCOVA, Sidak's Post-hoc; * Difference of medians T1-T0 (interquartile range), Kruskal-wallis test, Dunn's Post-hoc;
a,b Different letters on the lines indicate that the difference between
groups was statistically significant (p≤0.05); partial η2 = effect size.
Discussion
The results of this study showed that the group of elderly
women who received conventional proprioceptive training
improved mobility, balance, and physical performance, and
reduced the concern with the fear of falling. The group that
underwent training with virtual reality showed improvement in
all the outcomes of the study, with the exception of functional
mobility. The control group did not show improvement in any of
the study outcomes, and mobility showed a statistically significant worsening after the period studied.
The positive effects of the training sessions proposed in this
study are probably due to the characteristics of the proprioceptive activities developed. The activities involved integrated
movements in several dimensions, including joint acceleration,
strength, neuromuscular efficiency, the adaptation of several
components of the nervous system, allowing gains in proprioception, strength, and muscular endurance, as well as flexibility,
motor coordination, and balance [34-36].
Some authors have defended in their studies the importance
of specific training to improve functionality and prevent falls
in the elderly [36-39]. The trainings approached by the aforementioned authors were similar to the present study and had
similar results. However, differently from those studies, which
compared only two groups and approached a smaller number
of outcomes, the present study, besides assessing several outcomes at the same time, such as mobility, balance, functional
performance and fear of falling, compared three groups, being
two training modalities and a control group.
The effects of a training with conventional multisensorial
exercises on balance, mobility and physical performance of elderly people, observed, at the end of the intervention period, a
shorter time to perform the TUGT and a better physical performance of the lower limbs evaluated by the SPPB [11]. According
to some studies, the better performance on the TUGT obtained
by the conventional training group reflects better conditions
to perform daily activities, such as standing up, sitting down,
walking, among others; and consequently, a lower probability
of falls, institutionalization and even death in elderly individuals
[40,41].
The improvement in the functional performance of the
lower limbs obtained by the group who did conventional training, in the present study, can be explained by the sensory and
musculoskeletal stimuli offered by the sensory-motor training
of this modality. These exercises are performed with alternating
speeds, thus stimulating different types of muscle fibers, among
them type II, which help improve speed when performing the
movement of sitting down and getting up from a chair [11].
Another clinical trial analyzed balance and the risk of falls
in two groups of elderly subjects, one participating in a conventional balance circuit and the other as a control. The results
showed improvements in balance and a reduction in the risk of
falls in the intervention group in relation to the control group
[37]. A 12-month randomized clinical trial that compared the effects of a conventional balance program with the control group
in elderly women observed that only the group that received
conventional training improved functional balance, increasing
on average 5 points in the BBS score, and reduced the number
of falls [42]. However, in both studies, the conventional training was not compared with another type of intervention, which
makes it impossible to generalize the results and compare the effects with other interventions.
Another study that analyzed the effects of a conventional
multi-sensory proprioceptive exercise program on the functionality of the elderly was, in which they observed a significant improvement in balance (BBS) and functional mobility (TUGT) of
community-dwelling elderly people [43]. It is worth noting that
the results were not compared with another type of training or
with a control group, which makes it impossible to compare the
effects with another intervention.
The effects of a conventional balance exercise circuit on several functional variables in elderly women showed the program
promoting improvements in balance and functional performance of elderly women compared to the control group. In addition, the high compliance of the participants with the training
illustrates the importance of programs that incorporate socialization and exercises that are similar to the activities of daily
living [38]. However, conventional training was not compared
with another intervention modality.
The training strategies adopted for the proper functioning
of the center of mass within the base of support of the elderly
in different positions, maintenance of proper body alignment,
maintenance of gaze stability, adequate anticipatory and reactive reactions to external disturbances, functional exercises and
with changes in support surfaces, activate proprioceptive impulses integrated to sensory-motor centers that automatically
control the adjustments in the contraction of postural muscles,
providing improvement in postural balance and functionality to
the elderly [44,45]. In the present study, the conventional training program adopted used similar techniques, which helped
achieve the objectives.
Regarding training using virtual reality, the positive effects
obtained in the functionality and fear of falling of the elderly
women in this study can be explained by the characteristics
made available by this resource, such as a higher number of
repetitions, high variability, auditory and visual feedback, besides the complexity of the virtual tasks with high cognitive and
motor demands, which helps to promote a higher integration of
this type of skills, contributing to a greater independence in the
daily life of these individuals [46-48].
In another randomized clinical trial that investigated the effect of the Xbox Kinect on elderly individuals, it was concluded
that the group that used virtual reality showed positive results
in the improvement of gait, lower limb muscle strength, and
balance when compared to the control group that did not perform any activity [14]. Another study that evaluated the effects
of training with Xbox Kinect [49] also observed that the group
submitted to virtual reality significantly increased the BBS score
when compared to the control group. However, the results of
these studies were not compared with another intervention,
which makes it impossible to generalize the results and compare the effects with a conventional intervention.
Another virtual reality-based physical exercises protocol, observed an improvement in mobility and physical performance
in the elderly. The authors believe that these improvements are
attributed to neurobiological mechanisms that may have improved efficiency in cognitive and spatial navigation skills [50].
It was also observed that regarding fear of falling, the findings
were not significant, but the exergame group obtained better
scores compared to the control group, showing a positive outlook.
The concern with the fear of falling in elderly people exponentially limits the performance of habitual tasks that demand
multiple interactions of the sensory-motor system [4]. Elderly
individuals with functional capacity, balance and gait alterations end up having impairments in the execution of a safe
and effective ambulation and compromise the self-confidence
of these individuals in avoiding falls, generating a basis for the
construction of the fear of falling [5]. Although few studies have
approached the effects of specific physical therapy training on
the fear of falling in elderly people, the present study showed
that not only the conventional and virtual training had positive effects on the elderly females' fear of falling, but they also
contributed to the improvement of factors related to the fear
of falling, such as the physical performance of the lower limbs,
mobility, and balance.
Regarding the comparisons of the intergroup effects on the
outcomes studied, the results of the present study showed that
there was a better effect of conventional training and exergame
when compared to the control group, but no significant differences between the intervention groups.
When comparing the effects of balance exercises with virtual
reality and conventional balance exercises in the elderly, they
showed that in both groups, the scores for balance (BBS) and
mobility (TUGT) improved significantly as time, but the changes
were similar between the two groups [51]. Regarding fear of
falling (FES-I), there were no changes after the treatment period
in both trainings. In the study that compared the effects of virtual reality through the Xbox Kinect versus conventional physical therapy in the elderly, they observed that both interventions
had positive effects on balance, gait, and cardiorespiratory fitness of the elderly, but there were no significant differences between the training modalities [39]. It is worth mentioning that,
unlike the present study, in both of the aforementioned studies
the intervention groups were not compared with a passive control group, i.e., that did not receive any type of intervention.
The results of the present study showed that both the conventional training and the training with virtual reality provided
improvement in the functionality and fear of falling of the elderly women. The efficacy of the training shown in this study
proves that the improvement of elderly women's functionality
can be achieved without costly and easily accessible resources
as in the case of conventional training; and that virtual reality
has become an available resource, providing, through an innovative therapy, benefits to the functionality of elderly women
because of the playfulness and various possibilities of tasks to
be performed through the proposed games.
It is important to emphasize the need for follow-up studies
in order to verify the duration of the effects of the interventions
after their completion.
Conclusion
The results of this study showed that conventional proprioceptive training and virtual reality-based training can promote
improved functionality and reduced fear-of-fall concerns in elderly women; however, when comparing the intergroup effects,
there were no significant differences between the trainings with
respect to the outcomes studied.
References
- Sousa SEM, Oliveira MCC. Viver a (e para) aprender: uma intervenção-ação para promoção do envelhecimento ativo. Rev Bras Geriatr Gerontol. 2015; 8: 405-415.
- Locks RR, Costa TC, Koppe S, Yamaguti AM, Garcia MC, et al.
Effects of strength and flexibility training on functional performance of healthy older people. Rev Bras Fisioter. 2012; 16: 184-
190.
- Ruzene JR, Navega MT. Assessment of balance, mobility and
flexibility in active and sedentary elderly women. Rev Bras Geriatr Gerontol. 2014; 17: 785-793.
- Borges VS, Silva NS, Malta AC, Xavier NC, Bernardes LES. Falls,
muscle strength, and functional abilities in community-dwelling
elderly women. Fisioter Mov. 2017; 30: 357-366.
- Cruz DT, Duque RO. Leite ICG. Prevalence of fear of falling, in
a sample of elderly adults in the community. Rev Bras Geriatr
Gerontol. 2017; 20: 309-318.
- Lustosa LP, Silva JP, Coelho FM, Pereira DS, Parentoni NA, et al.
Effect of a muscular resistance program on the functional capacity and muscle strength of the knee extensors in pre-frail community-dwelling elderly women: a randomized crossover clinicatrial. Rev Bras Fisioter. 2011; 15: 318-324.
- Silva MF, Goulart NBA, Lanferdini FJ, Marcon M, Dias CP. Relationship between levels of physical activity and quality of life of
sedentary and physically active elderly. Rev Bras Geriatr Gerontol. 2012; 15: 635-642.
- Howe TE, Rochester L, Neil F, Skelton DA, Ballinger C. Exercise for
improving balance in older people. Cochrane Database Syst Rev.
2011; 11.
- Bird M, Hill KD, Ball M, Hetherington S, Williams AD. The longterm benefits of a multi-component exercise intervention to
balance and mobility in healthy older adults. Arch Gerontol
Geriatr. 2011; 52: 211-216.
- Kuptniratsaikul V, Praditsuwan R, Assantachai P, Ploypetch T,
Udompunturak S, et al. Effectiveness of simple balancing training program in elderly patients with history of frequent falls. Clin
Interv Aging. 2011; 6: 111-117.
- Alfieri FM, Riberto M, Gatz LS, Ribeiro CPC, Battistella LR. Uso de
testes clínicos para verificação do controle postural em idosos
saudáveis submetidos a programas de exercícios físicos. Acta fisiatr. 2010; 17: 153-158
- Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S,
et al. Interventions for preventing falls in older people living in
the community. Cochrane Database Syst Rev. 2012; 12: 1-44.
- Nematollahi A, Kamali F, Ghanbari A, Etminan Z, Sobhani S. Improving balance in older people: a double-blind randomized
clinical trial of three modes of balance training. J Aging Phys Act.
2016; 24: 189-195.
- Sato K, Kuroki K, Saiki S, Nagatomi R. Improving walking, muscle
strength, and balance in the elderly with an exergame using kinect: a randomized controlled trial. Games Health J. 2015; 4:
161-167.
- Karahan AY, Tok F, Taşkın H, Kuçuksaraç S, Başaran A, et al. Effects
of exergames on balance, functional mobility, and quality of life
of geriatrics versus home exercise programme: randomized controlled study. Cent Eur J Public Health. 2015; 23.
- Lee M, Son J, Kim J, Yoon B. Individualized feedback-based virtual reality exercise improves older women’s self-perceived
health: a randomized controlled trial. Arch Gerontol Geriatr.
2015; 61: 154-160.
- Lai CH, Peng CW, Chen YL, Huang CP, Hsiao YL, et al. Effects of
interactive video-game based system exercise on the balance of the elderly. Gait Posture. 2013; 37: 511-515.
- Rendon AA, Lohman EB, Thorpe D, Johnson EG, Medina E, et al.
The effect of virtual reality gaming on dynamic balance in older
adults. Age Ageing. 2012; 41: 549-552.
- Schulz KF, Altman DG, Moher D, Consort G. CONSORT 2010
statement: updated guidelines for reporting parallel group randomised trials. J Clinic Epidemiol. 2010; 340: c332.
- World Health Organization (WHO). Global recommendations on
physical activity for health. Geneva: World Health Organization,
2010.
- Folstein MF, Folstein SE, Mchugh PR. Mini-Mental State: a practical method for grading the cognitive state of patients for clinician. J Psychiatr Res. 1975; 12: 189-198.
- Bertolucci PHF, Brucki SMD, Campacci SR, Juliano Y. The Mini-Mental State Examination in a general population: impact of
education. Arch Neuropsiquiatr. 1994; 52: 1-7.
- Santos AA, Bertato FT, Montebelo MIL, Guirro ECO. Effect of proprioceptive training in diabetic women. Rev Bras Fisioter. 2008;
12: 183-187
- Alfieri FM. Distribution of plantar pressure in the elderly after
proprioceptive intervention. Rev Bras Cineantropom Performance Hum. 2008; 10: 137-142.
- Rezende AAB, Silva IL, Beresford H, Batista LA. Evaluation of the
effects of a sensorimotor program on the gait pattern of elderly
women. Physioter Move. 2012; 25: 317-324.
- Khoshelham K, Elberink SO. Accuracy and resolution of kinect
depth data for indoor mapping applications. Sensors. 2012; 12:
1437-1454.
- Miyamotto ST, Junior IL, Berg KO, Ramos LR, Natour J. Brazilian
version of the Berg balance scale. Braz J Med Biol Res. 2004; 37:
1411-1421.
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of functional mobility elderly persons. J Am Geriatr Soc. 1991; 39: 142-
148
- Nakano MM. Brazilian version of the Short Physical Performance
Battery – SPPB: Cultural Adaptation and Reliability Study [dissertation]. Campinas: State University of Campinas, 2007.
- Camargos FFO, Dias RC, Dias JMD, Freire MTF. Cross-cultural adaptation and evaluation of the psychometric properties of the
Falls Efficacy Scale – International in Brazilian elderly (FES-I-BRASIL). Rev Bras Fisioter. 2010; 14: 37-43.
- Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs.
Front Psychol. 2013; 4: 863
- Murphy KR, Myors B, Wolach A. Statistical power analysis: a simple and general model for traditional and modern hypothesis
tests. 4 ed. New York: Routledge/Taylor & Francis Group, 2014.
- Cohen J. Statistical power analysis for the behavioral sciences. 2
ed. Hillsdale, NJ: Lawrence Earlbaum Associates, 1988.
- Farias J, Scatambul T, Silva F, Faria W, Santos C, et al. Effect of
eight weeks of functional training on the physical fitness of elderly people. Rev Acta Bras Mov Hum. 2014; 4: 13-27.
- Magalhães AL, Cruz AL, Reis NS. Balance and functional mobility tests in predicting and preventing the risk of falls. Rev Bras
Geriatr Gerontol. 2015; 18: 129-140.
- Pereira LM, Gomes JC, Bezerra IL, Oliveira LS, Santos MC. Functional training impact on balance and elderly functionality not
institutionalized. Rev Bras Ci Mov. 2017; 25: 79-89.
- Costa J, Avelar B, Gonçalves C, Pereira M, Safons M. Effects of
the balance circuit on functional balance and the possibility of
falls in elderly women. Motricity. 2012; 8: 485-492.
- Avelar BP, Costa JN, Safons MP, Dutra MT, Bottaro M, Gobbi S, et
al. Balance exercises circuit improves muscle strength, balance,
and functional performance in older women. Age Ageing. 2016;
38: 1-11.
- Bacha JMR, Gomes GCV, Freitas TB, Viveiro LAP, Silva KG, et al.
Effects of kinect adventures games versus conventional physical therapy on postural control in elderly people: a randomized
controlled trial. Games Health J. 2018; 7: 24-36.
- Nascimento FA, Vareschi AP, Alfieri FM. Prevalence of falls, associated factors and functional mobility in institutionalized elderly.
Arch Cat Med. 2008; 37: 7-12.
- Alfieri FM, Carreres MAA, Figuera RG, Battistella LR. Comparison of the execution time of the Timed up and go (TUG) test in
the elderly with and without a history of falls. Rev Esp Geriatric
Gerontol. 2010; 45: 174-175
- Madureira MM, Bonfá E, Takayama L, Pereira RMR. A 12-month
randomized controlled trial of balance training in elderly women with osteoporosis: Improvement of quality of life. Maturitas,
2010; 66 : 206-211.
- Souza LA, Fernandes AB, Patrizzi LJ, Walsh IAP, Shimano SGN.
Effects of supervised multisensory training for six weeks on balance and quality of life in elderly people. RMRP. 2016; 49: 223-
231
- Cruz A, Oliveira E, Melo S. Biomechanical analysis of equilibrium
in the elderly. Rev Acta Ortop Bras. 2010; 18: 96-99.
- Lopes MN, Passerini CG, Travensolo CF. Effectiveness of a physiotherapeutic protocol for balance in institutionalized elderly. Rev
Cienc Biol e Saúde. 2010; 31: 143-152.
- Deutsch JE, Borbely M, Filler J, Huhn K, Guarrera-Bowlby P. Use
of a low-cost, commercially available gaming console (Wii) for
rehabilitation of an adolescent with cerebral palsy. Phys Ther.
2008; 88: 1196-2207.
- Pompeu JE, Mendes FA, Silva KG, Lobo AM, Oliveira TP, et al.
Effect of Nintendo Wii™-based motor and cognitive training on
activities of daily living in patients with Parkinson’s disease: a
randomised clinical trial. Physiotherapy. 2012 ; 98 : 196-204.
- Mendes FAS, Arduini L, Botelho A, Cruz MB, Santos-Couto-Paz
CC, et al. Patients with Parkinson’s Disease are able to improve
their performance in virtual Xbox Kinect® tasks: “a case series”.
Motricity. 2015 ; 11 : 68-80.
- Bieryla KA. Xbox Kinect training to improve clinical measures of
balance in older adults: a pilot study. Aging Clin Exp Res. 2015;
28: 451-457.
- Monteiro-Junior RS, Figueiredo LFS, Maciel-Pinheiro PT, Abud
ELR, Engedal K, et al. Virtual reality–based physical exercise with
exergames (physex) improves mental and physical health of institutionalized older adults. J Am Med Dir Assoc. 2017; 18: 454.
e1-454.e9.
- Yeşilyaprak SS, Yıldırım MŞ, Tomruk M, Ertekin O, Algun ZC.
Comparison of the effects of virtual reality-based balance exercises and conventional exercises on balance and fall risk in older
adults living in nursing homes in Turkey. Physiother Theory and
Pract. 2016; 32: 191-201.