Clinical & Medical Surgery
Open Access
Volume 3
Yingyong Suksathien*; Pattawat Chuvanichanon; Thanut Tippimanchai; Jithayut Sueajui; Satja Thoedpraisan
*Corresponding Author: Suksathien Y
Department of Orthopaedic Surgery, Maharat Nakhon Ratchasima Hospital, Chang Phueak Rd, Mueang District, Nakhon Ratchasima Province 30000, Thailand.
Tel: 0-4423-5529; Email: ysuksathien@yahoo.com
Article Info
Received: Dec 20, 2022
Accepted: Jan 19, 20233
Published: Jan 27, 2023
Archived: www.jclinmedsurgery.com
Copyright: © Suksathien Y (2022).
Abstract...
Introduction: Femoral morphology can have significant impact on leg-length discrepancy (LLD) when using conventional cementless stems in Dorr’s type A. The impact when using short stem is not well known, therefore, this study aimed to analyze the difference in LLD between Dorr’s type A&B femurs, and to define the risk factors for significant LLD in short stems.
Materials and method: The digitized radiographs of 208 consecutive unilateral short stem THA were retrospectively reviewed. LLD, femoral cortical index (FCI), femoral neck resection level, femoral, acetabular, and hip offsets were evaluated. A threshold of LLD > 7 mm was defined as significant LLD. The subsidence threshold of more than 3 mm was defined as clinically significant.
Results: The mean LLD was 4.44 mm. (-13.41-14.07, 4.4). There was no statistically significant difference of LLD and femoral neck resection level between Dorr’s type A&B cases, p=0.406 and p=0.18 respectively, whereas there was significantly higher LLD in cases with femoral neck resection level >5 mm when compared with <5 mm (p=0.01). Sixty-five hips (31.3%) had significant LLD, univariate and multivariate regression analysis demonstrated that age, Dorr’s type A, BMI had no significant influence on significant LLD, whereas neck resection level >5 mm did have a statistically significant influence, (OR 2.20; 95% CI, 1.2-4.0; p=0.01) and (OR 2.4; 95% CI 1.3-4.4; p=0.007) respectively. There was significantly lower LLD in cases with femoral resection level 2-3 mm when compare with >3.1 mm (p<0.001), with no difference in significant subsidence (p=0.97). There was no stem revision in this study.
Conclusions: Proximal femoral morphology was not influenced on LLD when using short stems. Nevertheless, neck resection level >5 mm did have a statistically significant influence with significant LLD. Neck resection level 3 mm should be more suitable for Asian patients.
Citation: Suksathien Y, Chuvanichanon P, Tippimanchai T, Sueajui J, Thoedpraisan S. Does Femoral Morphology Impact on Leg-Length Discrepancy when using Short Stem Cementless Total Hip Arthroplasty?. J Clin Med Surgery. 2023; 3(1): 1069.
Introduction
Total Hip Arthroplasty (THA) is one of the most performed and successful procedures to date. Post-operative leg length equality is highly desirable but is challenging to achieve. Post-operative Leg-Length Discrepancy (LLD) is associated with pain, limping, and patient dissatisfaction [1,2]. Many previous studies have demonstrated that femoral morphology can have a significant impact on post-operative LLD, particularly notable when using conventional cementless femoral stems with metaphyseal fixation in Dorr’s type A femurs [3-7], which increased the risk of osteointegration failure and implant loosening [8-10].
Short stem THAs are commonly used in young and active patients, and have shown excellent results in patients with osteonecrosis of the femoral head (ONFH) [11-13] and developmen- tal dysplasia of the hip (DDH) [14] in our previous studies. The advantages of these stems include more proximal load transfer which reduces stress shielding, thigh pain, and they provide better options should revision surgery become necessary [15]. The Metha stem is designed for metaphyseal anchorage within the cortical ring of the femoral neck with no diaphyseal invasion [16], therefore, this stem should not be influenced by proximodistal dimensional mismatch in Dorr’s type A femur [3]. Few publications have studied post-operative LLD in the short stems and their risk factors; due to different areas of fixation, they might demonstrate different patterns than with the conventional stems.
The purpose of this study was to analyze the difference in LLD between Dorr’s type A and B femurs and to define the risk factors for significant LLD in short stem THAs, including any radiographic parameters. We hypothesize that femoral morphology in Dorr’s type A would not have a significant impact on LLD when using short stems.
Materials and methods
We conducted this study after approval from our hospital’s Institutional Review Board (107/2021). The digitized radiographs of 231 patients with unilateral hip disease who had undergone unilateral short stem THA in our institute between February 2011 and August 2020 were retrospectively reviewed. The inclusion criteria were patients aged >18 years with unilateral hip disease with good bone quality (Dorr’s type A and B) [3]. Excluded from this study were (1) 3 patients with a 3 cm or longer LLD before THA, (2) 4 patients with DDH, (3) 4 patients with proximal femoral deformity, and (4) 12 patients with prior hip surgery, leaving 208 patients to study.
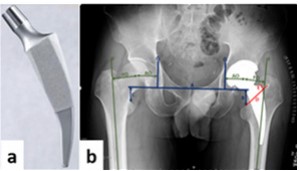
All THAs in this study were performed using Metha short stem by three experienced senior surgeons (YS, JS, ST) through a modified Hardinge approach. The final stem was selected intraoperatively by each surgeon’s decision, based on the maximal impingement-free range of motion, optimal soft-tissue tension without dislocation or subluxation, and most balanced LLD. The Metha short stem is cementless, tapered, collarless, monobloc, and made of titanium forged alloy (Ti6A14V) with suggested metaphyseal anchorage within the closed ring of the femoral neck (Figure 1a). This stem is available in 5 sizes (0, 1, 2, 3, and 4) and 3 caput-column-diaphysis (CCD) angles (120o, 130 o and 135 o). The Metha short stem is round coated with Plasmapore, a calcium phosphate layer for inducing osseointegration. In all cases the femoral neck was cut above the notch of the femoral neck at an angle of 50o to the femoral axis to create a closed cortical ring [17]. Intra-operative calcar cracks that occurred incidentally were routinely treated with cerclage wire.
The Metha short stem was classified as type IIA according to Khanuja et al [18]; type I is femoral neck only, type II is calcar loading, type III is calcar loading with lateral flare, and type IV is shortened tapered stem. Additionally, type 2 stems are subdivided into 4 subtypes: A, trapezoidal; B, round; C, threaded; and D, thrust plate. The cementless acetabular cup (Plasmafit, B.Braun Aesculap, Tuttlingen, Germany) with polyethelene liner (Vitelene, Vit E Stabilized Highly Crosslinked Polyethelene, B.Braun Aesculap, Tuttlingen, Germany) and metal head were used in all cases. The acetabular cup was aimed at the anatomical hip center with the target angles for acetabular cup abduction and anteversion of 40° and 15° respectively in all hips. The diameter of the femoral head depended on cup size; 32 mm for cup diameter 50 mm or less, and 36 mm for cup diameter 52 mm or more.
Patients were allowed to stand and progress to full weight-bearing using crutches on the second post-operative day. The standard protocol for Anteroposterior (AP) digital radiograph of both hips with both legs at 15° internal rotation and lateral cross-table, to control femoral stem rotation, was taken on the first post-operative day and at each follow-up radiograph. Patients were routinely contacted every three months in the first post-operative year and then every six months thereafter.
Proper pre-operative radiographs were assessed by using the femoral cortical index (FCI), as per Dorr et al [3], of which: >0.6 were Dorr’s type A, ≤0.6 and ≥0.5 were Dorr’s type B, and <0.5 were Dorr’s type C. On the first proper post-operative AP digital radiographs which were calibrated with known femoral head size to minimize magnification error, the LLD was defined as the perpendicular distance between the upper border of the lesser trochanters and a horizontal reference line connecting the inferior aspect of the acetabular teardrops (inter-teardrop line). Values were reported with reference to the native con- tralateral hip, with positive values indicating lengthening and negative values indicating shortening of the operated side. The line from the upper border of the lessor trochanter to the notch of the femoral neck was defined as the base of the femoral neck level. The distance from the most lateral point of the femoral neck cut perpendicular to the base of the femoral neck level in millimeters was defined as the femoral neck resection level. The hip Center of Rotation (COR) was defined using a circular tool determining the femoral head diameter and its center. Acetabular Offset (AO) was calculated as the distance from the COR to the perpendicular line on the inter-teardrop line. Femoral offset (FO) was calculated as the distance from the COR perpendicular to the proximal Femoral Shaft Axis (FSA). Hip offset (HO) was calculated as the sum of AO and FO (Figure 1b). According to Fujita et al [19], the LLD threshold of 7 mm was considered as reasonable threshold for reducing the residual discomfort post-operatively, therefore, the cut-off point for the absolute value of post-operative LLD >7 mm was defined as significant LLD in this study. Stem subsidence was calculated as the different distance from the shoulder point of the stem to the most prominent point of the greater trochanter between the first post-operative day and at minimum one year follow-up by AP radiograph [20].
The subsidence threshold of more than 3 mm was considered as clinically significant subsidence [21,22].
Two independent observers (PC,TT) measured each radiograph, and measurements were averaged into one final value after confirming that data reliability between the observers was sufficient. For the intra-observer, the results of Intraclass Correlation Coefficients (ICCs) of the observer 1 for FCI, LLD, femoral neck resection level, FO and AO of operated and contralateral hips were 0.91 (95% CI 0.87-0.94), 0.84 (95% CI 0.77-0.88), 0.89 (95% CI 0.84-0.82), 0.91 (95% CI 0.86-0.94), 0.89 (95% CI 0.83- 0.93), 0.87 (95% CI 0.80-0.92) and 0.86 (95% CI 0.78-0.91) respectively. The results of the observer 2 were 0.89 (95% CI 0.86- 0.93), 0.9 (95% CI 0.86-0.93), 0.9 (95% CI 0.86-0.93), 0.9 (95% CI 0.85-0.94), 0.85 (95% CI 0.77-0.90), 0.88 (95% CI 0.82-0.92) and 0.84 (95% CI 0.76-0.90) respectively. For the inter-observer, the results were 0.85 (95% CI 0.79-0.89), 0.71 (95% CI 0.6-0.79), 0.77 (95% CI 0.68-0.83), 0.85 (95% CI 0.77-0.9), 0.75 (95% CI 0.61-0.84), 0.83 (95% CI 0.74-0.89) and 0.78 (95% CI 0.66-0.86) respectively.
Statistical analysis
According to the results of previously published data about post-operative LLD which compared Dorr’s type A and type B femurs [6], 44% of Dorr’s type A femurs gained more than 5 mm of leg length; this was 30% more likely to be 5 mm long when compared to Dorr’s type B femur (p=0.029). Power calculations revealed that 87 cases were required in each group in variability with 90% power.
The mean, standard deviation, lowest and highest values were used in the descriptive statistics of data. Demographic data between Dorr’s type A and type B femurs were compared using Chi-squared test. The unpaired t-test was used to compare LLD and femoral neck resection level between Dorr’s type A and type B cases, between femoral neck resection level >5 and <5 mm, >3.1 and 2-3 mm cases, and values of FO, AO, and HO between operated and native contralateral hips. Univariate and multivariate regression analysis were used to identify the factors related to significant LLD including age (>55 yrs.), Dorr’s type A, body mass index (BMI) (>30 kg/m2) and femoral neck resection level (>5 mm) [17]. SPSS version 25.0 (SPSS Inc., Chicago, IL) was used for all statistical analyses with p < 0.05 defined as statistically significant.
Results
A total of 208 hips, 140 males (67.3%) and 68 females (32.7%) were included in the final analysis. The mean age was 50.3 years (18-77, 11.8) with a mean BMI of 24.1 (14.7-40.9, 4.5). There were 100 cases (48.1%) of Dorr’s type A and 108 cases (51.9%) of Dorr’s type B. The diagnosis included 169 cases (81.2%) of osteonecrosis of the femoral head (ONFH), 21 cases (10.1%) of primary osteoarthritis of the hip and 18 cases (8.7%) of femoral neck fracture. Stem size 0 was used in 82 cases (39.4%), size 1 in 57 cases (27.4%), size 2 in 49 cases (23.6%), size 3 in 18 cases (8.7%), and size 4 in 2 cases (0.9%). Stems with CCD angle 120o, 130o and 135o were used in 20 (9.6%), 64 (30.8%), and 124 (59.6%) cases respectively. There was no statistical difference in demographic data between Dorr’s type A and B groups (Table 1). The mean LLD was 4.44 mm. (-13.41-14.07, 4.4) and the mean femoral neck resection level was 4.86 mm (2.08-11.84, 2.1) for the entire cohort. In Dorr’s type A cases, the mean LLD and the mean femoral neck resection level were 4.62 mm. (-13.41-14.07, 4.3) and 5.06 mm (2.08-11.84, 2.1). In Dorr’s type B cases, the mean LLD and the mean femoral neck resection level were 4.28 mm. (-8.71-12.6, 4.6) and 4.66 mm (2.2- 10.87, 2.04). There was no statistically significant difference in LLD and femoral neck resection level between Dorr’s type A and type B cases, p=0.406 and p=0.18, respectively (Table 2). Sixty-five hips (31.3%) had significant LLD (>7 mm) with a mean of 9.4 mm. (7.12-14.07), including 32 cases (49.2%) of Dorr’s type A and 33 cases (50.8%) of Dorr’s type B. The univariate regression analysis demonstrated that age, Dorr’s type A, and BMI had no major influence on significant LLD, whereas neck resection level (> 5 mm) did have a statistically significant influence (OR 2.20; 95% CI, 1.2-4.0; p=0.01) (Table 3). The multivariate regression analysis also demonstrated that neck resection level (> 5 mm) did have a statistically significant influence (OR 2.4; 95% CI 1.3-4.4; p=0.007). The intra-operative calcar crack incidence was 8.2% (17/208) and all were treated with cerclage wire with no further subsidence. The mean LLD for the entire cohort of the femoral neck resection level >5 mm was 5.46 mm. (-8.39-14.07, 4.39), and for femoral neck resection level <5 mm was 3.75 mm (-13.41-12.77, 4.35), a statistically significant difference (p=0.01). The mean LLD of the neck resection level >3.1 mm was 5.61 mm (-8.71-12.77, 3.43) and for femoral neck resection level 2-3 mm was 2.7 mm (-13.41-10.74, 4.51), a statistically significant difference (p<0.001) (Table 4). There were 5 cases with significant subsidence (>3 mm), 4 cases (2.40%) in neck resection level >3.1 mm and 1 case (2.44%) in neck resection level 2-3 mm groups, with no significant difference (p=0.97). There was no stem revision in this study. In operated hips, the mean FO was 33.12 mm. (10.68-56.57, 8.2), the mean AO was 31.74 mm (24.35-43.43, 3.7) and the HO was 64.86 mm (41.7-88.41, 8.9). In the native contralateral hip, the mean FO was 30.1 mm (11.43-49.47, 7.6), the mean AO was 31.42 mm (23.23-41.28, 3.3) and the mean HO was 61.52 mm (41.64-82.48, 8.2). There was no statistically significant difference in FO, AO and HO between the operated hips and the native contralateral hips, p-values 0.97, 0.15 and 0.98 respectively.Table 1: Demographic data.
| Parameters | Entire cohort | Dorr’ type A | Dorr’ type B | p-value |
|---|---|---|---|---|
| No. of hips | 208 | 100 | 108 | |
| Gender (male/female) | 140/68 | 70/30 | 70/38 | 0.42 |
| Mean age (years)(range,SD) | 50.3 (18-77,11.8) | 48.7 (18-73,11.6) | 51.7 (23-77,11.9) | 0.07 |
| Mean BMI (range,SD) | 24.1 (14.7-40.9,4.5) | 23.8 (14.7-35.8,4.5) | 24.4 (16-40.9,4.4) | 0.4 |
| Diagnosis (cases)(%) | ||||
| ONFH | 169 (81.2%) | 83 (83%) | 86 (79.6%) | 0.53 |
| Primary osteoarthritis of the hip | 21 (10.1%) | 11 (11%) | 10 (9.3%) | 0.68 |
| Femoral neck fracture | 18 (8.7%) | 6 (6%) | 12 (11.1%) | 0.19 |
| Stem size (cases) (%) | 0.13 | |||
| 0 | 82 (39.4%) | 645 (45%) | 37 (34.3%) | |
| 1 | 57 (27.4%) | 29 (29%) | 28 (25.9%) | |
| 2 | 49 (23.6%) | 21 (21%) | 28 (25.9%) | |
| 3 | 18 (8.7%) | 5 (5%) | 13 (12%) | |
| 4 | 2 (0.9%) | 0 | 2 (1.9%) | |
| CCD angle (cases) (%) | 0.71 | |||
| 120o | 20 (9.6%) | 10 (10%) | 10 (9.3%) | |
| 130o | 64 (30.8%) | 28 (28%) | 36 (33.3%) | |
| 135o | 124 (59.6%) | 62 (62%) | 62 (57.4%) |
BMI, body mass index (kg/m2); ONFH, osteonecrosis of the femoral head; CCD, caput-column-diaphysis
p-value: Dorr’s type A vs. Dorr’s type B.
Table 2: Results of leg-length discrepancy (LLD) and femoral neck resection level in the entire cohort and in Dorr’s type A & B. Data presented as mean (mm) (range, SD).
| Parameters | Entire cohort (208) | Dorr’ type A (100) | Dorr’ type B (108) | p-valuea |
|---|---|---|---|---|
| Leg-length discrepancy (LLD) | 4.44 (-13.41-14.07,4.4) | 4.62 (-13.41-14.07, 4.3) | 4.28 (-8.71-12.6, 4.6) | 0.406 |
| Femoral neck resection level (>5 mm) | 4.86 (2.08-11.84, 2.1) | 5.06 (2.08-11.84, 2.1) | 4.66 (2.2-10.87, 2.04) | 0.18 |
a p-value: Dorr’s type A vs. Dorr’s type B.
Table 3: Results of univariate regression analysis.
| Variables | Univariate analysis | ||
|---|---|---|---|
| OR | 95% CI | p-value | |
| Age (>55 yrs.) | 1.6 | 0.9-3.0 | 0.1 |
| Dorr’s type A | 1.2 | 0.7-2.2 | 0.503 |
| BMI (>30 kg/m2) | 0.6 | 0.3-1.6 | 0.359 |
| Femoral neck resection level(>5 mm) | 2.2 | 1.2-4.0 | 0.01 |
OR, odds ratio; Bold indicates significant value.
Table 4: Results of leg-length discrepancy (LLD) in the entire cohort of any femoral neck resection levels. Data presented as mean (mm) (range, SD).
| Parameters (cases) | Values | p-value |
|---|---|---|
| > 5 mm (84) (mean 7 mm (5.01-11.84)) | 5.46 (-8.39-14.07, 4.39) | 0.1 |
| < 5 mm (124) (mean 3.4 mm (2.08-4.97)) | >3.75 (-13.41-12.77, 4.35) | |
| > 3.1 mm (167) (mean 5.55 mm (3.11-11.84) | 5.61 (-8.71-12.77, 3.43) | <0.001 |
| 2-3 mm (41) (mean 2.63 mm (2.08-3.07) | 2.7 (-13.41-10.74, 4.51) |
Bold indicates significant value.
Table 5: Summary of post-operative LLD in different types of short stem.
| Authors | Femoral stem | Khanuja et al [18] classification | LLD(mm) | Number |
|---|---|---|---|---|
| Schmidutz et al [27] | Metha, Aesculap, Germany | 2A | 3.3 (-10-14, 5.3) | 50 |
| Confalonieri et al [28] | Metha, Aesculap, Germany | 2A | 4.1 (0-7, 1.7) (navigation) 7.9 (3-14, 2.8) (manual) | 44 |
| This study | Metha, Aesculap, Germany | 2A | 4.44 (-13.41-14.07, 4.4) | 208 |
| Amenabar et al [29] | Nanos, Smith&nephew, Germany | 2A | 0.36 | 147 |
| Kutzner et al [30] | Optimys, Mathys AG, Switzerland | 2B | 1.2 (-10-10,3.3) | 114 |
| Kim et al [31] | Proxima, DePuy, UK | 3 | 3.1 (-5-5, 1.0) | 84 |
| Innmann et al [32] | Fitmore, Zimmer, Warsaw, IN | 4 | 0.8 (-10-15, 3.2) | 100 |
| Luger et al [33] | Fitmore, Zimmer, Warsaw, IN | 4 | 1.11 + 5.13 | 117 |
Bold indicates significant value.
Discussion
Achieving post-operative leg length equality is a challenging procedure in THA. There is a broad consensus that less than 10 mm of post-operative LLD is clinically acceptable [23,24]. The perception of LLD after THA is one of the most common sources of patient dissatisfaction and can have a direct influence on the considered success of the operation. Sykes et al [25] reported that discrepancies >5 mm were likely to be perceived. In a recent study, Fujita et al [19] demonstrated that an LLD threshold of 7 mm was considered reasonable for reducing the residual discomfort following THA.
Femoral neck resection level was not a significant risk factor for higher post-operative LLD in any of the conventional implants [5,26], whereas many previous studies have demonstrated that the femoral morphology can have significant impact on post-operative LLD, particularly notable when using conventional cementless femoral stems with metaphyseal fixation in Dorr’s type A femurs [3-7], which increased the risk of osteointegration failure and implant loosening [8-10]. Boese et al [4] revealed that proximal femoral anatomy of a relevant proportion of adult hips was not adequately covered by standard femoral components; 28.9% of cases were mismatched. Brumat et al [5] used a conventional cementless metaphyseal fixation stem (Implantcast-EcoFit) and, reported that higher canal flare index (CFI) was an independent risk factor for post-operative LLD > 5 mm with an odds ratio of 4.5 (p=0.03). Lim et al [6] demonstrated that high femoral cortical index (FCI) increased the risk of lengthening (p=0.017) and low FCI increased the risk of shortening (p=0.005). Mavčič et al [7] in their literature review concluded that higher FCI and/or CFI (corresponding to Dorr’s type A with narrow distal medullary canal) increases the risk of leg lengthening after THA, osseointegration failure and implant loosening, particularly in conventional metaphyseal fixation stem. Ishii et al [8] demonstrated that suboptimal radiological changes were detected in cases with greater distal fill and smaller proximal fill in the narrow femoral canal of Asian patients using proximally coated taper wedge stem. Park et al [9] showed that stem survivorship of Dorr’s type A femur (97.8%) was lower than that of type B femur (99.5%) (p=0.041) using taper wedge stem at a minimum follow-up of 5 years. Warth et al [10] demonstrated that failure to optimize canal fill with appropriate surgical technique using taper wedge stem predisposes femoral components to failure from aseptic loosening.
In this study, we found no statistically significant difference of LLD between Dorr’s type A and type B cases (p=0.406), while the femoral neck resection level between two groups was also showed no statistically significant difference (p=0.18). Our finding demonstrated that this stem was not influenced by proximodistal dimensional mismatch when used in Dorr’s type A fe- mur, as the Metha stem is designed for metaphyseal anchorage within the cortical ring of the femoral neck with no diaphyseal invasion.
The mean LLD for the entire cohort in this study was 4.44 mm. (-13.41-14.07, 4.4), a finding consistent with Schmidutz et al [27], who demonstrated a mean LLD of 3.3 mm. (-10-14, 5.3) using Metha stem. Confalonieri et al [28] also showed the mean LLD of 4.1 mm. (0-7, 1.7) and 7.9 mm. (3-14, 2.8) using Metha stem with navigation and manual techniques respectively. Different results of LLD were reported from many previous studies using different types of short stem according to Khanuja et al [18] [27-33] (Table 5).
It is particularly important to identify risk factors intraoperatively to predict significant post-operative LLD (>7 mm.) when using Metha stem, which would be useful for choosing the proper surgical technique. In this study we found that the only significant influencing factor for significant post-operative LLD was femoral neck resection level >5 mm; univariate and multivariate regression analysis showed statistical significance, (OR 2.20; 95% CI, 1.2-4.0; p=0.01) and (OR 2.4; 95% CI 1.3-4.4; p=0.007) respectively. Restoration of limb length seems to be more challenging with short stem THA, as it tends to increase limb length, which is related to the femoral neck resection level. In the present study we found significantly higher LLD when the femoral neck resection level was >5 mm when compared with <5 mm (p=0.01). The femoral neck resection level of about 5 mm was recommended for primary metaphyseal fixation in Caucasian patients using Metha stem [17]. Femoral morphology of Asian patients is relatively small when compared with Caucasians, and the femoral neck is generally smaller and shorter; therefore, the femoral neck resection level in Asian patients should be shorter than Caucasian patients. In this study we found significantly lower LLD when the femoral neck resection was 2-3 mm when compared with >3.1 mm (p<0.001). To create the cortical ring of the femoral neck, essential for Metha stem fixation, while preventing significant LLD post-operatively, neck resection level 3 mm should be more suitable for Asian patients. Therefore, the distance from the notch of the femoral neck to the neck resection level should be accurately measured using the depth gauge before performing femoral neck resection.
Nevertheless, operating surgeons need to balance between optimal soft tissue tension and post-operative LLD, always keeping in mind that achieving equal leg length after THA is only a secondary goal in comparison to rigid fixation of components in the bone, and joint stability [34]. In this study we found that FO and HO increased in the operated hip compared to native contralateral hip, which correlated with positively increased strength of the abductor muscles, and improved the biomechanical reconstruction of the hip when using Metha stem.
Press-fit is one of the key factors for stability of cementless stems. The surgeon is guided by visual, sensory, and auditory clues during insertion of the short stem; a good balance between perfect press-fit level and not fracturing the calcar remains challenging. In this study, the incidence of intra-operative calcar crack was 8.2% (17/208) and all cases were treated with cerclage wire without complication. We believed this was because of the relatively narrow neck diameter of patients in our country, reflected by the most commonly used size being 0 (39.4%), and 70.6% of calcar crack cases used size 0. As in our previous study, Suksathien et al [12] reported 4.8% rate of intra-operative calcar crack using Metha short stem in patients with ONFH without any complication at a minimum follow-up of 5 years.
Limitations
This study had some limitations. First, acetabular cup position may affect the post-operative LLD, nevertheless, to minimize acetabular variability, we excluded patients with DDH. Second, due to the radiological study design, no post-operative clinical data was obtained. Third, our cohort was a consecutive study of Metha stem, which was classified as type IIA according to Khanuja et al [18]; the surgical technique for femoral neck resection might be different from type I, III and IV. Finally, our cohort was relatively small and was from a single institute; different results might have been obtained by different surgeons with varying levels of experience in any type of short stem THA.
Conclusion
Proximal femoral morphology in Dorr’s type A femur was not influenced on LLD when using Metha stem. Nevertheless, femoral neck resection level did influence post-operative LLD, and neck resection level >5 mm did have a statistically significant influence with significant LLD, which should be taken into consideration when performing femoral neck resection. To diminish LLD, while creating an effective closed ring of the femoral neck for rigid stem fixation, neck resection level 3 mm should be more suitable for Asian patients.
Declaration
Conflict of interest: All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Funding sources:None.
Acknowledgement:The authors wish to acknowledge Dr. Urawit Piyapromdee MD, for assisting with the statistical analysis and gratefully thank Mr. Jason Cullen for the careful proof-reading of the manuscript.
References
- Roder C, Vogel R, Burri L, Dietrich D, Staub LP. Total hip arthroplasty: leg length inequality impairs functional outcomes and patient satisfaction. BMC Musculoskelet Disord. 2012; 13: 95.
- Plaass C, Clauss M, Ochsner PE, Ilchmann T. Influence of leg length discrepancy on clinical results after total hip arthroplasty-a prospective clinical trial. Hip Int. 2011; 21: 441-449.
- Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, et al. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993; 14: 231-242.
- Boese CK, Dargel J, Jostmeier J, Eysel P, Frink M, et al. Agreement Between Proximal Femoral Geometry and Component Design in Total Hip Arthroplasty: Implications for Implant Choice. J Arthroplasty. 2016; 31: 1842-1848.
- Brumat P, Pompe B, Antolič V, Mavčič B. The impact of canal flare index on leg length discrepancy after total hip arthroplasty. Arch Orthop Trauma Surg. 2018; 138: 123-129.
- Lim YW, Huddleston JI, Goodman SB, Maloney WJ, Amanatullah DF. Proximal Femoral Shape Changes the Risk of a Leg Length Discrepancy After Primary Total Hip Arthroplasty. J Arthroplasty. 2018; 33: 3699-3703.
- Mavčič B, Antolič V. Cementless femoral stem fixation and leg-length discrepancy after total hip arthroplasty in different proximal femoral morphological types. Int Orthop. 2021; 45: 891- 896
- Ishii S, Homma Y, Baba T, Ozaki Y, Matsumoto M, et al. Does the Canal Fill Ratio and Femoral Morphology of Asian Females Influence Early Radiographic Outcomes of Total Hip Arthroplasty With an Uncemented Proximally Coated, Tapered-Wedge Stem? J Arthroplasty. 2016; 31: 1524-1528.
- Park CW, Eun HJ, Oh SH, Kim HJ, Lim SJ, et al. Femoral Stem Survivorship in Dorr Type A Femurs After Total Hip Arthroplasty Using a Cementless Tapered Wedge Stem: A Matched Comparative Study With Type B Femurs. J Arthroplasty. 2015; 34: 527-533.
- Warth LC, Grant TW, Naveen NB, Deckard ER, Ziemba-Davis M, et al. Inadequate Metadiaphyseal Fill of a Modern Taper-Wedge Stem Increases Subsidence and Risk of Aseptic Loosening: Technique and Distal Canal Fill Matter! J Arthroplasty. 2020; 35: 1868-1876.
- Suksathien Y, Sueajui J. The short stem THA provided promising results in patients with osteonecrosis of the femoral head. J Med Assoc Thai. 2015; 98: 768-774.
- Suksathien Y, Sueajui J. Mid-term results of short stem total hip arthroplasty in patients with osteonecrosis of the femoral head. Hip Int. 2019; 29: 603-608.
- Suksathien Y, Suarjui J, Ruangboon C, Akkrasaeng T. Mid-term results of short versus conventional cementless femoral stems in patients with bilateral osteonecrosis of the femoral head. Eur J Orthop Surg Traumatol. 2021.
- Suksathien Y, Tippimanchai T, Akkrasaeng T, Ruangboon C. Midterm results of short-stem total hip arthroplasty in patients with Crowe type I and II developmental dysplasia of the hip. Eur J Orthop Surg Traumatol. 2021; 31: 319-325.
- Floerkemeier T, Schwarze M, Hurschler C, Gronewold J, Windhagen H, et al. The Influence of Tribological Pairings and Other Factors on Migration Patterns of Short Stems in Total Hip Arthroplasty. Biomed Res Int. 2017; 8756432.
- Floerkemeier T, Gronewold J, Berner S, Olender G, Hurschler C, et al. The influence of resection height on proximal femoral strain patterns after Metha short stem hip arthroplasty: an experimental study on composite femora. Int Orthop. 2013; 37: 369-377.
- Khanuja HS, Banarjee S, Jain D, Pivec R, Mont MA. Short bone conserving stems in cementless hip arthroplasty. J Bone Joint Surg Am. 2014; 96: 17421752.
- Fujita K, Kabata T, Kajino Y, Tsuchiya H. Optimizing leg length correction in total hip arthroplasty. Int Orthop. 2020; 44: 437-443.
- Jahnke A, Wiesmair AK, Fonseca CA, Ahmed GA, Rickert M, et al. Outcome of short- to medium-term migration analysis of a cementless short stem total hip arthroplasty using EBRA-FCA: a radiological and clinical study. Arch Orthop Trauma Surg. 2020; 140: 247-253.
- Kim YH, Kim JS, Joo JH, Park JW. A prospective short-term out-come study of a short metaphyseal fitting total hip arthroplasty. J Arthroplasty. 2012; 27: 88-94.
- Albers A, Aoude AA, Zukor DJ, Huk OL, Antoniou J, et al. Favorable Results of a Short, Tapered, Highly Porous, Proximally Coated Cementless Femoral Stem at a Minimum 4-Year Follow-Up. J Arthroplasty. 2016; 31: 824-829.
- McWilliams AB, Grainger AJ, O’Connor PJ, Redmond AC, Stewart TD, Stone MH. A review of symptomatic leg length inequality following total hip arthroplasty. Hip Int. 2013; 23: 6-14.
- Ng VY, Kean JR, Glassman AH. Limb-length discrepancy after hip arthroplasty. J Bone Joint Surg Am. 2013; 95: 1426-36.
- Sykes A, Hill J, Orr J, Humphreys P, Rooney A, et al. Patients’ perception of leg length discrepancy post total hip arthroplasty. Hip Int. 2015; 25: 452-456.
- Worlicek M, Weber M, Wörner M, Schwarz T, Zeman F, et al. The final implant position of a commonly used collarless straight tapered stem design (Corail®) does not correlate with femoral neck resection height in cement-free total hip arthroplasty: a retrospective computed tomography analysis. J Orthop Traumatol. 2018; 19: 20.
- Schmidutz F, Beirer M, Weber P, Mazoochian F, Fottner A, et al. Biomechanical reconstruction of the hip: comparison between modular short-stem hip arthroplasty and conventional total hip arthroplasty. Int Orthop. 2012; 36: 1341-1347.
- Confalonieri N, Manzotti A, Montironi F, Pullen C. Leg length discrepancy, dislocation rate, and offset in total hip replacement using a short modular stem: navigation vs conventional free-hand. Orthopedics. 2008; 31(10 Suppl 1).
- Amenabar T, Marimuthu K, Hawdon G, Gildone A, McMahon S. Total hip arthroplasty using a short-stem prosthesis: restoration of hip anatomy. J Orthop Surg (Hong Kong). 2015; 23: 90-94.
- Kutzner KP, Kovacevic MP, Roeder C, Rehbein P, Pfeil J. Reconstruction of femoro-acetabular offsets using a short-stem. Int Orthop. 2015; 39: 1269-1275.
- Kim YH, Kim JS, Park JW, Joo JH. Total hip replacement with a short metaphyseal-fitting anatomical cementless femoral component in patients aged 70 years or older. J Bone Joint Surg Br. 2011; 93: 587-592.
- Innmann MM, Spier K, Streit MR, Aldinger PR, Bruckner T, et al. Comparative Analysis of the Reconstruction of Individual Hip Anatomy Using 3 Different Cementless Stem Designs in Patients With Primary Hip Osteoarthritis. J Arthroplasty. 2018; 33: 1126-1132.
- Luger M, Hochgatterer R, Klotz MC, Allerstorfer J, Gotterbarm T, et al. A single-surgeon experience in reconstruction of femoro-acetabular offset and implant positioning in direct anterior approach and anterolateral MIS approach with a curved short stem. Arch Orthop Trauma Surg. 2021; 2.
- Piriou P, Bugyan H, Casalonga D, Lizée E, Trojani C, et al. Can hip anatomy be reconstructed with femoral components having only one neck morphology? A study on 466 hips. J Arthroplasty. 2013; 28: 1185-1191.