Clinical & Medical Surgery
Open Access
Volume 1
Macrì Giulia1*; Stefanizzi Gianluigi2; Cina Alessandro3; Mazzone Vincent Joseph4; Salgarello Marzia2
*Corresponding Author: Giulia Macrì
Largo Agostino Gemelli 8, 00168, Rome, Italy.
Email: giulia.macri@live.com
Article Info
Received: Dec 07, 2022
Accepted: Jan 18, 2023
Published: Jan 25, 2023
Archived: www.jclinmedsurgery.com
Copyright: © Macrì G (2022).
Abstract...
Dogs’ attacks are the most frequent cause (60-80%) of injuries inflicted by mammalian to humans. A multidisciplinary approach should be performed in patients with multiple bites or injuries that involve the deep tissues, especially with functional impairment at first examination.
We want to introduce a single case experience of a 64 years-old woman arrived at our emergency department for multiple lacerated and contused wounds of the head, sub-amputation of the right auricle, and laceration of the left one caused by a pit-bull attack.The greatest issue was the right auricle reconstruction that was apparently vital despite in continuity to the mastoid only with part of the lobe.
A complete bi-auricle reconstruction was performed with a total vital tissue sparing, introducing, furthermore, an intraoperative and postoperative controlled high-dose steroid therapy added to a mandatory antibiotic prophylaxis.We believe that an early but controlled steroid therapy could prevent the onset of severe edema that could compromise the already precarious vitality of the traumatized tissues preserved by the debridement.
Citation: Macrí G, Stefanizzi G, Cina A, Mazzone VJ, Salgarello M. Primary closure and steroid therapy in postoperative care of auricles reconstruction after severe dog bites injuries. J Clin Med Surgery. 2023; 3(1): 1068.
Introduction
Dogs’ attacks are the most frequent cause (60-80%) of injuries inflicted by mammalian to humans [1].
Children report more frequently head and neck wounds than adolescents and adults, whom bites involve usually extremities, especially arms [2].Wound management has been widely discussed in literature since 80s; early (<8 hours) medical and surgical treatment has been proven to be effective in reducing infections and scarring sequelae [1].
Firstly, a multidisciplinary approach (plastic surgeon, orthopedic surgeon, vascular surgeon) should be performed in patients with multiple bites or injuries that involve the deep tissues (muscles, tendons, neurovascular structures and bones, for example), especially with functional impairment at first examination.
Animal bites are obviously contaminated at different levels; some precautions should be taken into account to reduce the infection rate.
The first patient evaluation should assess the factors associated with a major infection risk including diabetes mellitus, immunosuppression, time of Emergency department (ED) presentation (greater than 6 to 12 hours for arm or legs or 12 to 24 hours for head and neck injuries), wound site (such as hand bite, involvement of venous and/or lymphatic structures) and bite agent (especially cats) [3].
A high pression irrigation of the wounds with saline or povidone-iodine solution is widely recommended to reach an adequate cleaning. In addition to abundant washing, an accurate exploration is then indicated in case of deep or extensive tissues laceration with a meticulous surgical debridement of mortified tissues; this practice further reduces the infection risk [4].
The most common antibiotic prophylaxis in dog bites is amoxicillin/clavulanate, 875/125 mg twice per day for 3 to 5 days [2].
We want to introduce a single case experience of a 64 yearsold woman arrived at our ED for multiple lacerated and contused wounds of the scalp, cheek, sub-amputation of the right auricle and laceration of the left one caused by a pit-bull attack (Figure 1). Deep and extensive lacerated wounds of the arms with loss of most of the muscles of the volar loggia of both.
No relevant comorbidities were identified. Tetanus and antibiotic prophylaxis were performed.
An exploration and debridement of the arms’ wounds was rapidly performed (<6 hours from ED arrival) by hand surgeons. An extensive lesion of the right brachial artery, associate with a devascularization of the arm, was detected and repaired with a graft from homolateral cephalic vein. No other vasculo-nervous lesions were detected bilaterally.
Plastic surgeons analyzed the head and neck lesions pro- ceeding with a primary, not serrated, closure of the wound after an accurate cleaning and surgical debridement.
The greatest issue was the right auricle reconstruction that was apparently vital despite in continuity to the mastoid only with part of the lobe. The removal of devitalized tissues was conducted with attention to preserve every single vital skin flap useful for an anatomic reconstruction. No local flaps or cartilage grafts were used.
Amoxicillin/clavulanate, 875/125 mg IV twice per day was continued during hospitalization in addition to dexamethasone, 8 mg IV twice per day for two days and, subsequently, with appropriate dose decreasing until 9 days. Dexamethasone avoided completely ears oedema that could compromise the labile vascularization. Neither infectious nor vascular complication occurred.
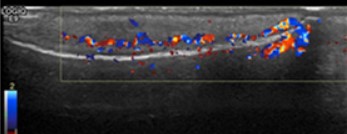
At the 14th postoperative day ears stiches were safely removed and at 30th day from the accident (Figure 2) a doppler ultrasound was performed to evaluate vascular supply of the sub-amputate ear. The inferior auricular vessel, from superficial temporal artery, was detected and an adequate vascularity of the auricle, on both sides of the cartilage, was confirmed by doppler ultrasound evaluation after 1-month from the surgery (Figure 3).
The first look to a severe injury, especially in visible sites or in case of deep and complex noble structures injuries, should not discourage the specialist to perform the best reconstruction in terms of safety, functionality, and aesthetic. A medical multidisciplinary post-operatory approach helps the good results of the surgery. The steroid therapy helps oedema reduction after an auricle severe injury, especially after a meticulous debridement, aimed at saving as many vital tissues as possible. Nevertheless, a trauma of this magnitude determines such a tissues mortification as to make them more susceptible also to physiological postoperative/post-traumatic oedema, which could lead to further devascularization especially in such delicate auricle’s tissues.
We believe that an early but controlled steroid therapy could prevent the onset of severe edema that could compromise the already precarious vitality of the traumatized tissues preserved by the debridement.
Declarations
Conflicts of interest: All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Funding sources: None.
Acknowledgment: None.
References
- Paschos NK, Makris EA, Gantsos A, Georgoulis AD. Primary closure versus non-closure of dog bite wounds. A randomised controlled trial. Injury. 2014; 45: 237-240.
- Ellis R, Ellis C. Dog and cat bites. Am Fam Physician. 2014; 90: 239-243.
- Cummings P. Antibiotics to prevent infection in patients with dog bite wounds: a meta-analysis of randomized trials. Ann Emerg Med. 1994; 23: 535-540.
- Morgan M, Palmer J. Dog bites. BMJ. 2007; 334: 413-417.