Clinical & Medical Surgery
Open Access
Volume 3
Yi Qiao; Xiaodong Wang; Yunfang Zhen; Jin Dai; Peng Ge*
*Corresponding Author: Peng Ge
Department of Pediatric Orthopedics, Children’s Hospital of Soochow University, No.92 Zhongnan Street, Indestrial Park, Suzhou, Jiangsu Province, China.
Tel: +86-0512-80692909; Email: 250453426@qq.com
Article Info
Received: Nov 26, 2022
Accepted: Jan 16, 2023
Published: Jan 24, 2023
Archived: www.jclinmedsurgery.com
Copyright: © Ge P (2023).
Abstract...
Objectives: FFemoral shaft fractures associated with multiple injuries are commonly encountered in school-age children. Clinical outcomes of non-surgical management of pediatric femoral shaft fractures with high-energy multiple injuries are not well characterized. In this study, we evaluated the early and mid-term clinical outcomes of non-surgical management of pediatric femoral shaft fractures with high energy multiple injuries in our setting.
Patients and methods: Retrospective review of school-age children with femoral shaft fractures managed non-surgically at the orthopedics department over a 3-year period.
Results: Eleven patients (6 boys and five girls; mean age: 7.2 years) with femoral shaft fractures associated with multiple injuries qualified the inclusion criteria. All fractures in this study population were sustained in road traffic accidents. Seven patients recovered very well. Basic functional recovery of lower limbs was satisfactory. Two patients had residual joint dysfunction, 4 patients showed abnormal gait, while 4 patients showed varying degrees of limp because of lower limb length discrepancy.
Conclusion: Clinical outcomes of non-surgical management of pediatric femoral shaft fractures at our center were comparable to the outcomes of other management approaches. Conservative management that shortens the duration of hospital stay without increasing cost of management should be encouraged.
Citation: Qiao Y, Wang X, Zhen Y, Dai J, Ge P. Early and Mid-Term Outcomes of Nonsurgical Management of Femoral Shaft Fractures with Associated Multiple Injuries in School-Age Children. J Clin Med Surgery. 2023; 3(1): 1067.
Introduction
Femoral shaft fracture is a common injury in children that accounts for about 33.7% of long bone fractures [1] and about 10% of all lower limb fractures [2]. It is most common in pre-school-age children (age <6 years) and the peak age at onset is approximately 5 years [3]. The ratio of male to female patients is approximately 3:1, and the late preschool period is another peak period of its occurrence [4,5]. The predominant cause of femoral shaft fracture in the early preschool period is low-energy injuries and most of these are simple femoral shaft fractures. However, in school-age children femoral shaft fractures are often caused by high-energy injuries, such as road traffic accidents or fall from height, and are often accompanied by compound injuries [6,7]. Femoral shaft fracture heals rapidly. Minimal overlap, angulation, or shortening tend to correct spontaneously with remodeling. Several studies have compared the clinical outcomes of conservative and surgical management of these fractures in school-age children [8,9]. However, there is no consensus on the optimal method for treatment of pediatric femoral fractures, especially with respect to long-term outcomes [8]. The selection of therapeutic modality between non-surgical treatment with home traction [10,11] and surgical management with internal or external fixation [12,13] is influenced by several factors, including age of the child, fracture site and location, associated trauma, surgical timing, and family circumstances [14,15].
Nonetheless, few studies have assessed the clinical outcomes of non-surgical management of pediatric femoral shaft fractures with high-energy multiple injuries. Therefore, in the present study, we evaluated the early and mid-term clinical outcomes of non-surgical management of pediatric femoral shaft fractures with high-energy multiple injuries in our setting.
Material and methods
This study was a retrospective analysis of all school-age children with femoral shaft fracture who were managed nonsurgically at the Orthopedics Department of the Children’s Hospital Affiliated to Soochow University between January 2015 and June 2017 (Table 1).
The inclusion criteria were: patients aged <15 years who presented with multiple trauma at the time of admission.
The exclusion criteria were: patients with osteogenesis imperfecta congenita, cerebral palsy, intra-articular or growth-plate fracture, pathological femoral shaft fractures (including bone cysts, metabolic bone disorders, or osteomyelitis), or open femoral shaft fractures. Data pertaining to the following baseline characteristics were extracted from the medical records: sex, age, parents’ occupation, schooling status, cause of femoral shaft fracture, time interval from fracture occurrence to presentation, and details of any associated injuries.
Table 1: Demographic and clinical characteristics of the study population.
| Case | Sex | Age (years) | Shock | Traction time (days) | Chest and abdominal injury | Head injury | Pelvic injury | Poly Fractures | Comminuted fractures |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Boy | 9 | Yes | 28 | Yes | Yes | Yes | No | Yes |
| 2 | Boy | 7 | Yes | 46 | No | No | No | Yes | Yes |
| 3 | Boy | 11 | Yes | 57 | No | No | yes | Yes | Yes |
| 4 | Girl | 5 | Yes | 28 | yes | yes | No | Yes | No |
| 5 | Girl | 5 | No | 28 | No | yes | No | Yes | Yes |
| 6 | Girl | 5 | No | 26 | Yes | yes | No | Yes | Yes |
| 7 | Boy | 6 | Yes | 23 | No | No | Yes | Yes | No |
| 8 | Boy | 6 | No | 33 | yes | No | Yes | Yes | Yes |
| 9 | Girl | 8 | No | 28 | No | Yes | No | Yes | No |
| 10 | Girl | 6 | No | 28 | No | No | Yes | No | No |
| 11 | Boy | 7 | No | 0 | No | No | No | Yes | Yes |
Therapeutic procedures
Femoral shaft fractures were confirmed by anteroposterior and lateral x-rays of the femur after patient resuscitation. The pattern was defined including site of fracture, degree of comminution, and displacement. Based on the site of the fracture, skin or bone traction was applied from the ankle to just above the knee. For children <3 years of age, skin traction is the commonly used method for treatment of femoral shaft fractures. For children >5 years of age, continuous and stable bone traction facilitates fracture reduction and maintenance of stability and tends to correct the angulation and shortening caused by muscle spasm.
Weights used for skin or bone traction depended on the age and weight of the patient. Weights of all school age children were determined by subtracting the weight of the mother from that measured while the mother carried the child in her arms. Clinically, we determined the exact amount of weight by gauging the length of the injured leg and comparing it with that of the uninjured limb. X-rays were reviewed weekly during hospitalization, and hip herringbone plaster fixation was performed after appearance of continuous and abundant callus on the x-rays. 4-6 weeks later, patients were gradually required to bear weight and walk according to the condition of fracture healing on x-rays. Bone traction was usually applied to the distal femur or proximal tibia with appropriate positioning. However, for some school-age children with life-threatening injuries to head, chest, abdomen, or pelvis, hip herringbone plaster fixation was performed in emergency. After the vital signs are stable, bone traction or surgical treatment would be carried out.
Results
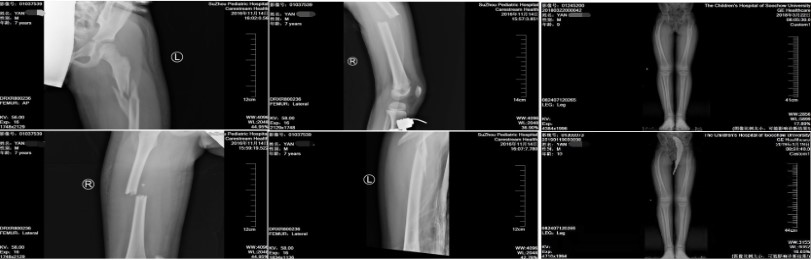
A total of 11 children [six boys and five girls; mean age: 7.2 years (range, 5-12)] qualified the selection criteria and were included in this study (Figures 1–4). All patients had sustained femoral shaft fracture in a road traffic accident. None of the patients were treated by one-stage surgery. The follow-up time ranged from 3 months to 45 months. During the follow-up period, strong healing with blurring or disappearance of the fracture line was observed on x-rays. None of the patients devel- oped pressure sores, infection, osteomyelitis, delayed healing, or nonunion (Table 2).
Seven patients had varying degrees of angulation deformity at the fracture end. Six patients had sagittal angulation while 2 patients had coronal angulation deformity. One patient developed redness and swelling around the nail canal. Two patients developed joint dysfunction, 4 patients had abnormal gait, while 4 patients had varying degrees of limp because of unequal length of lower limbs. Functional recovery was satisfactory in the remaining patients.
Seven patients recovered very well. However, the remaining 4 patients had slightly poor outcomes. Their details are summarized below.
Figure 2 shows the x-ray of a patient who presented with bilateral femoral shaft fracture with comminution of the left femoral shaft. Post-treatment residual length difference between the two lower limbs was approximately 0.5 cm and the patient walked with a limp (Figure 2). Figure 3 shows the x-ray of a patient who presented with fracture of different parts of the femur on both sides, and the right proximal femur had a comminuted fracture. Moreover, the limb length discrepancy was approximately 4 cm, and patient walked with a limp. Post-treatment, hip joint mobility was affected by hip varus deformity. Figure 1 shows the x-rays of a patient who presented with comminuted femoral shaft fracture with central nervous system injury. One year post-treatment, he showed limb shortening with healed deformity. In addition, there was overlapping and lateral angulation at the fracture site (Figure 1). Another patient had sustained a transverse fracture of the right femoral shaft. His right lower limb was shortened by approximately 0.5 cm with a sagittal angle of about 30° after one and a half years of treatment; the patient walked with a slight limp (Figure 4).
Table 2: Clinical outcomes in the study population.
| Case | Duration of follow-up (M) | Leg shortening | Limp | Pain | Range of motion | Sagittal angle | Coronal angle |
|---|---|---|---|---|---|---|---|
| 1 | 16 | Yes | Yes | No | Less | 20 | 25 |
| 2 | 26 | Yes | Yes | No | Good | 0 | 20 |
| 3 | 45 | Yes | Yes | Yes | Limited | 0 | 0 |
| 4 | 19 | Yes | yes | No | Good | 30 | 0 |
| 5 | 34 | No | No | No | Good | 10 | 0 |
| 6 | 30 | No | No | No | Good | 5 (Left) | 0 |
| 7 | 27 | No | No | No | Good | 0 | 0 |
| 8 | 14 | No | No | No | Good | 5 | 0 |
| 9 | 16 | No | No | No | Good | 0 | 0 |
| 10 | 17 | No | No | No | Good | 10 | 0 |
| 11 | 32 | No | No | No | Good | 0 | 0 |
Illustrative cases
Case 1: A 9-year-old boy suffered from central nervous system injury, epidural hemorrhage, contusion of both lungs and spleen, and fracture of the left femoral shaft. He was admitted to the ICU of our hospital. The child was delirious at admission, accompanied by acute central system damage and shock. His vital signs were: heart rate, 164 beats/minute; respiratory rate 30/minute; oxygen saturation (pulse oximetry), 84%; blood pressure, 110/64 mmHg. He was intubated and placed on ventilatory support. Blood transfusion and antibiotics were administered to maintain vital signs. Each department considered con- servative treatment after consultation. Femoral shaft fracture was treated with tibial tubercle bone traction. Eight days later, his vital signs gradually stabilized, and he was transferred to the common ward. Review x-ray showed satisfactory alignment and signs of callus formation. His parents requested conservative treatment. Finally, he was discharged from the hospital after plaster fixation (Figure 1).
Case 2: A 5-year-old girl sustained severe injuries in a road traffic accident which included lung contusion, spleen contusion, right femoral fracture, left supracondylar fracture of humerus, and multiple skin contusions. The girl was in shock at admission and was admitted to the ICU of our hospital. Her heart rate was 143 beats/minute and blood pressure was 96/55 mmHg, which gradually decreased to 79/47 mmHg. She was placed on ventilator support after endotracheal intubation. Symptomatic treatment such as blood transfusion and antibiotics were administered to maintain vital signs. After consultation with various departments, a conservative line of treatment was adopted. Tibial tubercle bone traction was applied for the right femoral fracture. Owing to gradual stabilization, she was transferred to the general ward after 13 days. X-ray showed callus formation at the fracture site. Since the operation time was lost, conservative treatment was continued. The patient was discharged after replacing plaster fixation at four weeks (Figure 4).
Discussion
Many therapeutic modalities have been developed for femoral shaft fractures sustained as part of high-energy multiple injuries in school-age children that can be treated conservatively or surgically. None of these approaches have yielded superior long-term clinical outcomes [8,6]. There is no consensus on the preferred management approach, although surgical procedures are increasingly used, especially for older children [8,17]. Usually, transverse fractures in children aged >6 years are treated using internal fixation with flexible intramedullary nails in the middle 60% of the femoral diaphysis [18,19]. Surgical treatment of femoral shaft fractures is resource intensive and is one of the most expensive trauma to manage in school-age children [20,21]. Financial constraints often lead to delay in surgical treatment of femoral shaft fractures, which increases hospitalization time before operation [22]. Moreover, surgical management of school-age children with femoral shaft fractures combined with high energy multiple injuries are not typically covered by health insurance. In addition, some of these patients are not suitable for surgical treatment or miss the optimum opportunity for surgery and have to receive conservative treatment. Lastly, some parents may themselves request conservative treatment [23]. Therefore, it is not surprising that skin traction is the most commonly used therapeutic modality for femoral shaft fractures in school age children in our setting. To the best of our knowledge, non-surgical management like early skin or bone traction followed by spica cast application is cost-effective and often the best method in school-age children [24-26]. In our study population, bone traction for patients aged >5 years was only used in patients who developed allergic reaction, plaster pressure sore, or skin infection due to extensive abrasions of their leg. Hip spica casting in our study population was utilized after a short period of bone or skin traction (generally 3 weeks). The use of hip spica casting was limited by the level of understanding of most parents, level of education, and their ability to treat a child with hip spica application at home. Early hip spica application has the advantage of overall lower cost of management and shorter length of hospital stay [11,27,28]. The major challenge and drawback of non-surgical management is the unequal length of lower limbs in our setting. It is the most common complication of femoral shaft fractures in children, mainly manifested as overgrowth [29]. Most of these cases develop limb length discrepancy in the first two years after the fracture, especially in the first three months; subsequently, it tends to disappear gradually within two years after the fracture. Some cases had growth disorder of the affected limb. The main reason was v-shaped epiphyseal injury, which caused premature epiphyseal closure and the formation of bone-bridge. There were 3 patients in this study, of which one patient with fracture of tibia and fibula had unequal length of lower limbs during follow up. This is likely attributable to the tendency of high energy injury to cause v-shaped epiphyseal injury, and muscle contraction causes shortening of the fracture end. Especially for comminuted fracture, the unstable fracture end increases the risk of shortening of the affected limb.A second challenge and drawback of non-surgical management is angulation and rotational deformity. For children aged 6–10 years, the coronal angle is <10°, sagittal angle is <15°, and it is shorter than 15 mm on the standard x-ray. However, for children older than 11 years, the coronal angle is <5°, the sagittal angle is <10°, and it is shorter than 10 mm. Rotational deformities cannot be corrected by themselves. Residual rotational deformities <10° generally do not affect the limb function. Considering that all the children in our study had multiple high energy injuries, some of them were treated with one-stage emergency bone traction because of the life–threatening injuries. By the time the vital signs of the children were stable, some of the fractures had healed abnormally, thus losing the opportunity for surgery. Therefore, the chance of adjusting the weight and direction of bone traction was lost. The incidence of angulation and deformity healing is relatively high for these children.
Conclusion
Owing to the life-threatening nature of high-energy injuries and the priority given to life support, the opportunity for surgical treatment of femoral shaft fractures may be lost in such patients. This increases the incidence of angulation deformity at the fracture site and the risk of limb length discrepancy and joint dysfunction. However, the joint function tends to recover well after functional exercises. To sum up, the clinical out-comes of non-surgical management of pediatric femoral shaft fractures in our environment is comparable to the outcome of other management approaches. Further randomized controlled studies are required to compare the clinical outcomes of non-surgical with those of surgical management of pediatric femoral shaft fractures.
Declarations
Availability of date and material: The datasets generated and analysed during the current study are available in the PACS system and available from the corresponding author reasonable request.
Funding: This study was funded by the clinical research funds (The new intervention strategies for the treatment of estrogen-induced avascular necrosis of femoral head BE2016674).
Authors’ contributions: Conceived and designed the experiments: Yi Qiao, Yunfang Zhen.
Performed the experiments: Yi Qiao, Xiaodong Wanga, Jin Dai, Yunfang Zhen.
Analyzed the data: Yi Qiao, Xiaodong Wanga, Jin Dai.
Wrote the paper: Yi Qiao, Xiaodong Wanga, Jin Dai.
References
- Landin LA. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950-1979. Acta Orthop Scand Suppl. 1983; 202: 1-109.
- Nwadinigwe CU, Ihezie CO, Iyidiobi EC. Fractures in children. Niger J Med. 2006; 15: 81-84.
- Staheli LT, Sheridan GW. Early spica cast management of femoral shaft fractures in young children. A technique utilizing bilateral fixed skin traction. Clin Orthop Relat Res. 1977; 162-166.
- Sinha SK, Kumar V, Singh A. Outcomes of fracture shaft femur in pediatric population managed at emergency. J Clin Orthop Trauma. 2017; 8: 313-319.
- AlKhatib N, Younis MH, Hegazy A, Ibrahim T. Early versus late treatment of paediatric femoral neck fractures: a systematic review and meta-analysis. Int Orthop. 2018.
- Flynn JM, Curatolo E. Pediatric femoral shaft fractures: a system for decision making. Instr Course Lect. 2015; 64: 453-460.
- Xu X, Lu X, Luo L, et al. [Effectiveness comparison of titanium elastic nail and locking compression plate fixation in treating femoral subtrochanteric fractures in older children]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017; 31: 1184-1189.
- Lebel E, Karasik M, Fisher D, Itzchaki M. [Treatment of pediatric femur fractures by immediate reduction and spica cast application clinical and economical feasibility in the Israeli medical system]. Harefuah. 2006; 145: 731-735.
- Zura R, Kaste SC, Heffernan MJ, et al. Risk factors for nonunion of bone fracture in pediatric patients: An inception cohort study of 237,033 fractures. Medicine (Baltimore). 2018; 97: e11691.
- Rapp M, Kaiser MM, Grauel F, et al. Femoral shaft fractures in young children (<5 years of age): operative and non-operative treatments in clinical practice. Eur J Trauma Emerg Surg. 2016; 42: 719-724.
- Scheerder FJ, Schnater JM, Sleeboom C, Aronson DC. Bryant traction in paediatric femoral shaft fractures, home traction versus hospitalisation. Injury. 2008; 39: 456-462.
- Narayanan UG, Hyman JE, Wainwright AM, et al. Complications of elastic stable intramedullary nail fixation of pediatric femoral fractures, and how to avoid them. J Pediatr Orthop. 2004; 24: 363-369.
- Flynn JM, Hresko T, Reynolds RA, et al. Titanium elastic nails for pediatric femur fractures: a multicenter study of early results with analysis of complications. J Pediatr Orthop. 2001; 21: 4-8.
- Poolman RW, Kocher MS, Bhandari M. Pediatric femoral frac- tures: a systematic review of 2422 cases. J Orthop Trauma. 2006; 20: 648-654.
- Melisie F, Krug E, Duijff JW, et al. [Age-specific treatment of femoral shaft fractures in children]. Ned Tijdschr Geneeskd. 2012; 156: A3976.
- Imam MA, Negida AS, Elgebaly A, et al. Titanium Elastic Nails Versus Spica Cast in Pediatric Femoral Shaft Fractures: A Systematic Review and Meta-analysis of 1012 Patients. Arch Bone Jt Surg. 2018; 6: 176-188.
- Flynn JM, Luedtke LM, Ganley TJ, et al. Comparison of titanium elastic nails with traction and a spica cast to treat femoral fractures in children. J Bone Joint Surg Am. 2004; 86: 770-777.
- Soleimanpour J, Ganjpour J, Rouhani S, Goldust M. Comparison of titanium elastic nails with traction and spica cast in treatment of children’s femoral shaft fractures. Pak J Biol Sci. 2013; 16: 391-395.
- Wright JG, Wang EE, Owen JL, et al. Treatments for paediatric femoral fractures: a randomised trial. Lancet. 2005; 365: 1153-1158.
- Heffernan MJ, Gordon JE, Sabatini CS, et al. Treatment of femur fractures in young children: a multicenter comparison of flexible intramedullary nails to spica casting in young children aged 2 to 6 years. J Pediatr Orthop. 2015; 35: 126-129.
- Wilson NC, Stott NS. Paediatric femoral fractures: factors influencing length of stay and readmission rate. Injury. 2007; 38: 931-936.
- Pape HC, Hildebrand F, Pertschy S, et al. Changes in the management of femoral shaft fractures in polytrauma patients: from early total care to damage control orthopedic surgery. J Trauma. 2002; 53: 452-461.
- Sangkomkamhang T, Thinkhamrop W, Thinkhamrop B, Laoha siriwong W. Incidence and risk factors for complications after definitive skeletal fixation of lower extremity in multiple injury patients: a retrospective chart review. F1000Res. 2018; 7: 612.
- Catena N, Senes FM, Riganti S, Boero S. Diaphyseal femoral fractures below the age of six years: Results of plaster application and long term followup. Indian J Orthop. 2014; 48: 30-34.
- Esenyel CZ, Ozturk K, Adanir O, et al. Skin traction in hip spica casting for femoral fractures in children. J Orthop Sci. 2007; 12: 327-333.
- Lee YH, Lim KB, Gao GX, et al. Traction and spica casting for closed femoral shaft fractures in children. J Orthop Surg (Hong Kong). 2007; 15: 37-40.
- Jauquier N, Doerfler M, Haecker FM, et al. Immediate hip spica is as effective as, but more efficient than, flexible intramedullary nailing for femoral shaft fractures in pre-school children. J Child Orthop. 2010; 4: 461-465.
- Gordon JE, Mehlman CT. The Community Orthopaedic Surgeon Taking Trauma Call: Pediatric Femoral Shaft Fracture Pearls and Pitfalls. J Orthop Trauma. 2017; 31: S16-S21.
- Dingemans SA, Sier MAT, Peters RW, et al. Two-stage treatment in patients with patients with high-energy femoral fractures does not lead to an increase in deep infectious complications: a propensity score analysis. Eur J Trauma Emerg Surg. 2018; 44: 125-131.