Clinical & Medical Surgery
Open Access
Volume 2
Urânia Fernandes1*; Gonçalo Guidi1; Daniela Martins1; Nádia Tenreiro2; Rita Marques2; João Pinto-de-Sousa3
*Corresponding Author: Urânia Fernandes
General Surgery Department, Hospital Centre Hospitalar de Trás-os-Montes e Alto Douro (CHTMAD), Clinical Academic Centre Trás-os-Montes e Alto Douro (CACTMAD), Rua dos Lagoeiros 43, 5000-508, Vila Real, Portugal.
Tel: +35-125-930-0500; Email: ufernandes@chtmad.min-saude.pt
Article Info
Received: Oct 25, 2022
Accepted: Nov 14, 2022
Published: Nov 22, 2022
Archived: www.jclinmedsurgery.com
Copyright: © Fernandes U (2022).
Abstract...
Introduction: Gurvits’ Syndrome or Acute Esophageal Necrosis (AEN) is an uncommon disease described as a “black esophagus” in Esophagogastroduodenoscopy (EGD). The prevalence is 0.2%, the incidence is less than 0.0125% and it is more common in elderly males with poor nutritional status and multiple comorbidities. The commonest clinical presentation is upper gastrointestinal bleeding (65%) but also epigastric or retrosternal pain and dysphagia. Mortality of AEN can achieve 32% and is often caused by comorbidities and infrequent complications (<11%). We present a clinical case and literature review about this rare entity.
Case report: A 81-year-old male presents to the emergency department with a 24-hour diffuse colicky abdominal pain and one episode of hematemesis, without hemodynamic repercussion or anemia. EGD revealed AEN extending to the gastric antrum, of unclear aetiology. During admission the patient presented persistent oral feeding intolerance due to esophageal stricture. He didn’t tolerate nasojejunal feeding, so a feeding jejunostomy was performed. After discharge the patient was submitted to endoscopic dilations with good results.
Discussion and conclusion: This case report describes an “extended” AEN complicated with esophageal stricture and oral feeding intolerance that imposed a surgical solution combined with an endoscopic approach. This rare entity that must be considered in differential diagnosis of upper gastrointestinal bleeding given its high mortality.
Citation: Fernandes U, Guidi G, Martins D, Tenreiro N, Marques R, et al. A Strange Case of Acute Esophageal Necrosis. J Clin Med Surgery. 2022; 2(2): 1059.
Introduction
Acute Esophageal Necrosis is an uncommon disease described as a “black esophagus” in Esophagogastroduodenoscopy (EGD). It was first described postmortem in 1967 by Brennan and in EGD by Goldenberg and colleagues in 1990. It is a rare entity more common in elderly males with poor nutritional status and multiple comorbidities. Its’ prevalence is 0.2% and incidence is less than 0.0125% in Caucasians’ endoscopic examinations [1].
Its aetiology is often not identified and is related to several comorbidities as diabetes mellitus, infections, hypercoagulable states, drugs, cardiovascular diseases, renal failure, antrum obstruction, trauma, alcoholism, malnutrition and advanced carcinomas. The most common clinical presentation is upper gastrointestinal bleeding (65%) but epigastric or retrosternal pain and dysphagia can also occur. Mortality of AEN can achieve 32% and is often caused by comorbidities and complications such as strictures (10.2%), mediastinitis/abscess (5.7%) and perforation (6.8%) [1,2,4].
The most probable pathophysiological mechanism of AEN is mucosa ischaemia. Distal esophagus is the poorest irrigated portion, fed by branches of left gastric artery. For this reason, it is the most susceptible area for ischemia and therefore where AEN is more frequently located. Another possible mechanism is antrum obstruction which causes gastro esophageal reflux, stasis and gastric distension. This is observed in AEN after alcoholic intoxication, long admissions or hiatal hernia with lower sphincteric dysfunction. Malnutrition can also be related with AEN by reducing mucosal barrier against gastric contents [1,3]. Diagnostic criteria of AEN are black esophagus with circumferential distribution; involvement of distal esophagus up to Esophagogastric Junction (EGJ); and no caustic ingestion. Histology usually reveals mucosal necrosis sometimes with sub mucosal extension and muscularis propria with highly inflammatory infiltration. Vascular thrombosis may also be present [1]. Gurvits and colleagues proposed a staging system for AEN progression based in endoscopic and histologic findings: stage 0 refers to a normal esophagus prior to necrosis; stage I describes a circumferentially black and friable esophagus up to EGJ; in stage II residual black mucosa may be present but white easily detachable exudates predominate, revealing pink friable mucosa; in stage III esophageal mucosa returns to its pink normal appearance [3].
Case report
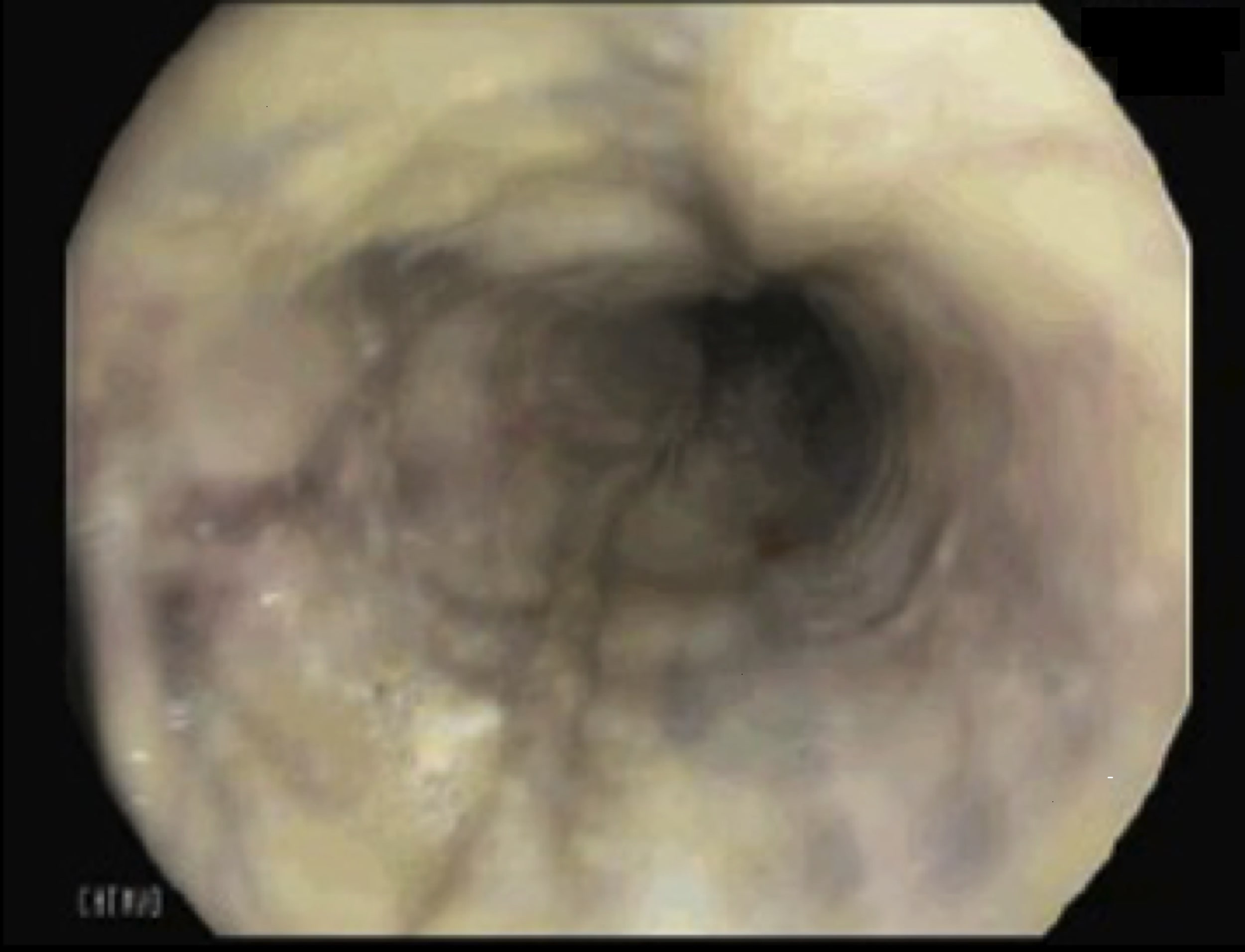
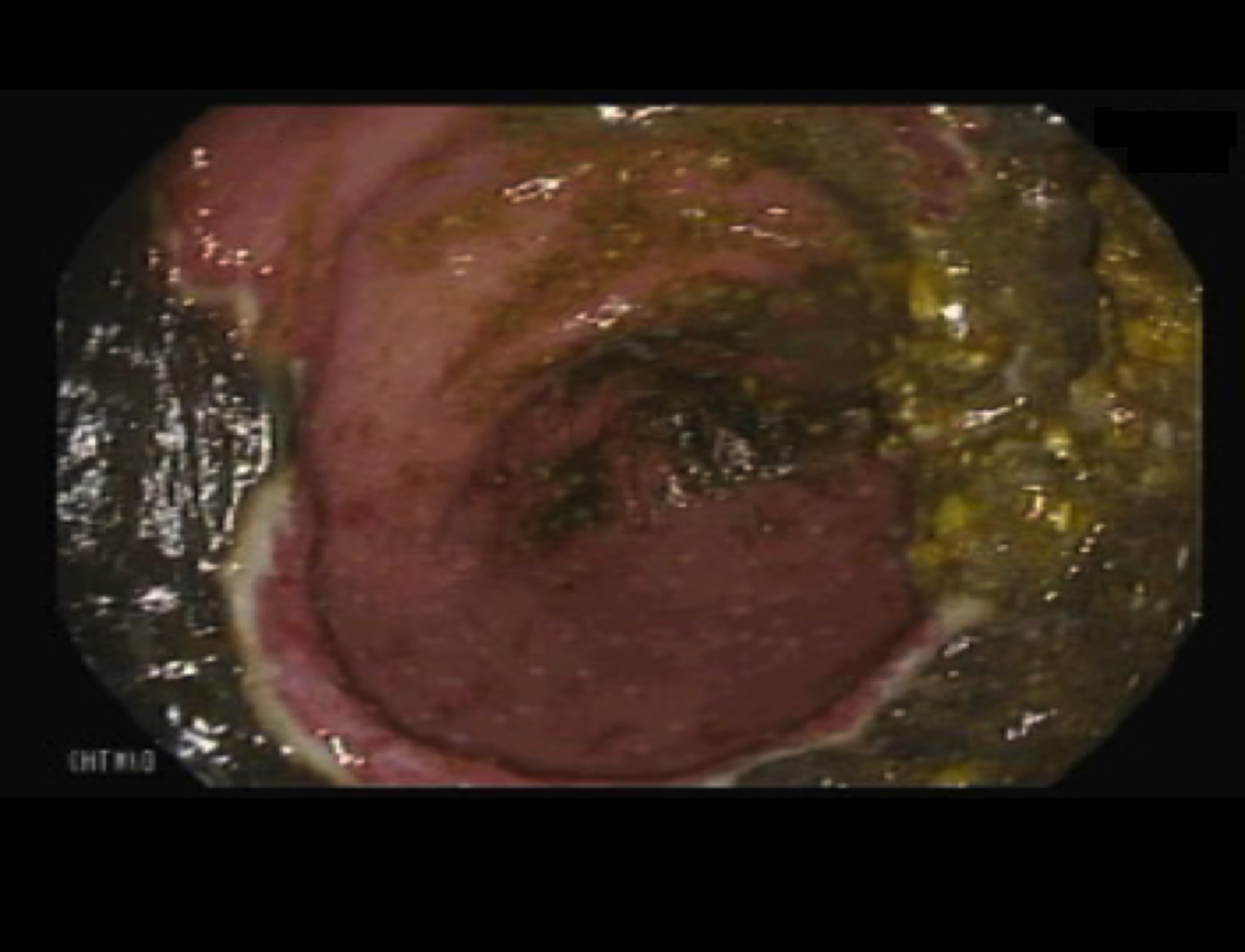
A 81-year-old male presented to the emergency department with a 24-hour diffuse colicky abdominal pain associated with one episode of hematemesis, dizziness and sweating. He denied altered bowel habits, fever, syncope, chest pain and as well as caustic and alcohol ingestion. Past medical history included Chronic Obstructive Pulmonary Disease and inguinal hernia surgery. He was hypertensive, tachycardic, without respiratory distress signs or altered mental status. Abdominal examination was painful to diffuse palpation without peritoneal signs or palpable masses with normal bowel sounds. Rectal examination was unremarkable as was abdominal x-ray. Laboratory work-up revealed elevated inflammatory markers and normal hemoglobin. EGD demonstrated “diffuse ulceration of proximal esophagus and distal black esophagus up to proximal antrum where there is a sudden transition to normal mucosa”, as shown in Figure 1 and Figure 2.
A Computed Tomography Angiography (CTA) revealed “distended esophagus without perforation; undefinition of gastric body and fundus’ wall, without peritoneal free air or fluid”, as shown in Figure 3. The patient was admitted and analgesics, sucralfate, proton pump inhibitors and empiric Piperacilin/ Tazobactam were initiated, as well as Fluconazole (for clinical diagnosis of oral and probable esophageal candidiasis). He initiated oral liquids intake, but progressively developed total oral feeding intolerance and contrast esophagography revealed a stricture in thoracic esophagus, confirmed by EGD. He could not tolerate nasojejunal feeding and a feeding Witzel jejunostomy was performed.
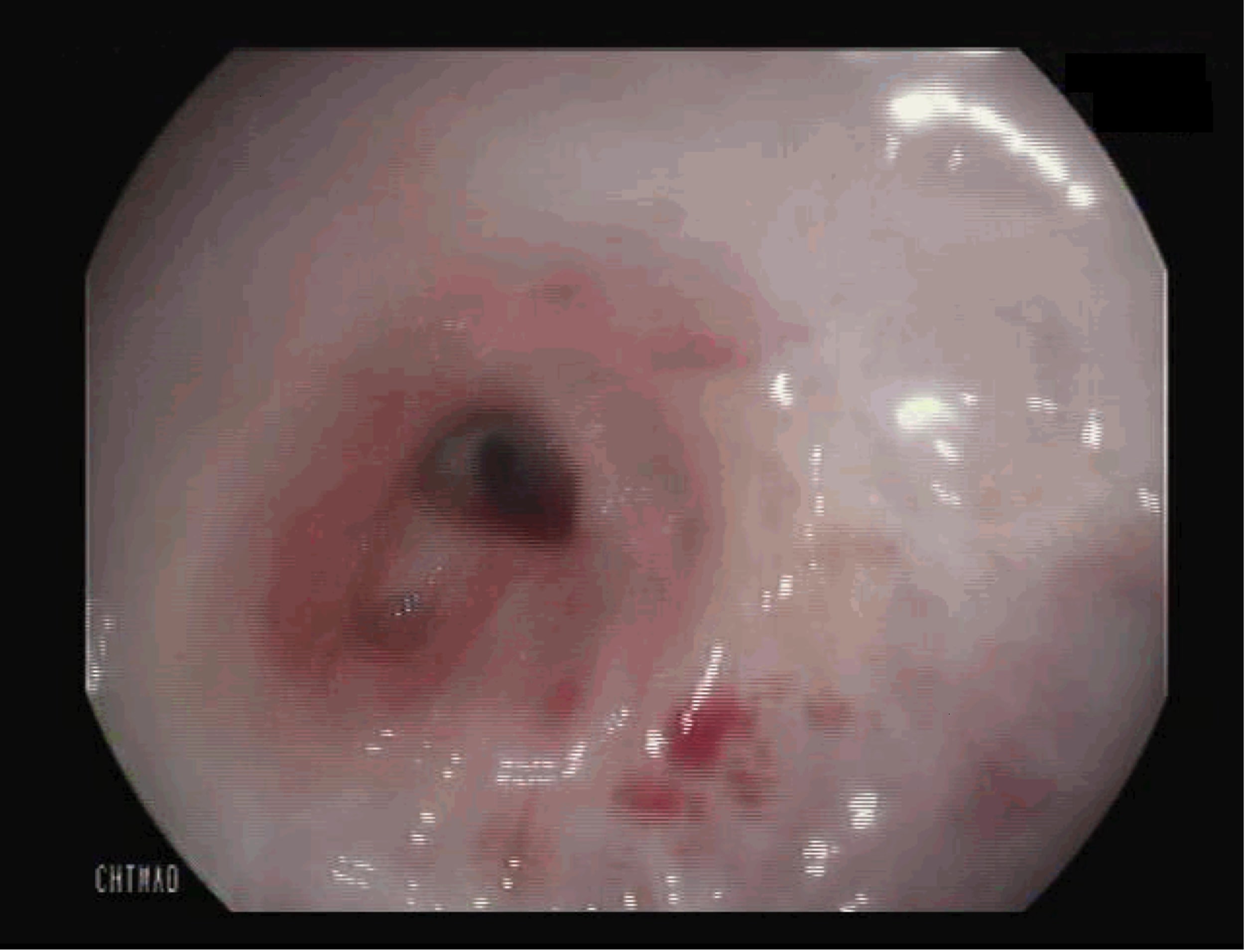
The patient did well in postoperative period, besides a left pneumonia treated with Meropenem, and was discharged 12 days later. After discharge he was submitted to serial ambulatory endoscopic dilations of the esophageal stricture shown in figure 4, with progressive oral tolerance for liquids. Unfortunately, the patient died with Fournier’s gangrene a few months later.
Discussion
This case report describes a rare entity. It is about AEN in an elderly male of unknown aetiology, which is in concordance with other series. In this case, AEN extended to gastric body and antrum, findings not described in literature, particularly without previous surgery, carcinoma, caustic ingestion, strangulated hiatal hernia or aorta dissection. According to the literature, some cases of proximal but not distal extension have been described [2]. Furthermore, this patient presented a well demarcated transition from ischemic to normal mucosa in the gastric antrum instead of EGJ, in contrast to that described by the diagnostic criteria. Probably the arterial supply of this patient was aberrant. It is noteworthy that referred esophageal candidiasis probably corresponded to stage II AEN as described by Gurvits and colleagues [3]. This patient had an extended AEN complicated with esophageal stricture and oral feeding intolerance that impelled a surgical solution, namely a feeding jejunostomy, considering it ́s comorbidities. Other treatment strategies options are endoscopic dilation (also performed in this case after discharge), injectable steroids and esophageal bypass [4]. Unfortunately, the patient died from another cause (Fournier’s gangrene), which is, to the best of our knowledge, non-related.
Conclusion
In conclusion, AEN is a rare entity that must be considered in differential diagnosis of upper gastrointestinal bleeding as a disease with high mortality.
References
- Zacharia GS, Sandesh K, Ramachandran T. Acute esophageal necrosis: an uncommon cause of hematemesis. Oman medical journal. 2014; 29: 302-304.
- Wu MH, Wu HY. Incremental change in acute esophageal necrosis: report of two cases. Surgery today. 2014; 44: 363-365.
- Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: a rare syndrome. Journal of gastroenterology. 2007; 42: 29-38.
- Sakatoku Y, Fukaya M, Miyata K, Nagino M. Successful bypass operation for esophageal obstruction after acute esophageal necrosis: a case report. Surgical case reports. 2017; 3: 4.