Clinical & Medical Surgery
Open Access
Volume 2
Jie Liu#; Jueling Liu#; Jian Xiong; Jingjing Xu; Xiao Luo1; Zeyu Zhu; Xialing Yang*; Yifeng Yu*; Nanye Wang
*Corresponding Author: Yifeng Yu & Xialing Yang
Associate professor of Ophthalmology, The Second Affiliated Hospital of Nanchang University, No. 1 Minde Road, Jiangxi 330000, China.
Tel: +86-13979180258, +86-13879187476; Email: 171018170@qq.com
Article Info
Received: Oct 21, 2022
Accepted: Nov 10, 2022
Published: Nov 17, 2022
Archived: www.jclinmedsurgery.com
Copyright: © Yu Y & Yang X (2022).
Abstract...
Aims: To observe the effect of micro-conjunctival auto grafting combined with amniotic membrane transplantation on the postoperative recurrence, complications and ocular surface symptoms among patients with recurrent pterygium.
Methods: A non-randomized controlled trial including 40 patients (43 eyes) with recurrent pterygium. The experimental group (n = 20, 21 eyes) received micro-conjunctival auto graft (2.0 mm × 3.0 mm) combined with amniotic membrane transplantation while the control group (n = 20, 22 eyes) was given conventional autologous conjunctival transplantation (depending on the area of the exposed sclera after the pterygium been removed). Except for postoperative recurrence, complications and pterygium size, ocular surface symptoms measured with Schirmer test I, partial ocular surface symptom score. Data were analyzed by SPSS version 24.0.
Results: Patients in the experimental group achieved a significant increase in foreign body sensation in 3 and 7 days after surgery (p < 0.05) than the control group. There was a decrease in Schirmer test I, burning sensation and pain, without statistical significance across different time point measurements at p < 0.05 between the groups. During the observational period, there was no recurrence and other serious complications.
Conclusions: These findings support the use of micro-conjunctival autografting combined with amniotic membrane transplantation for decreasing recurrence rate, damage to ocular surface and normal conjunctival tissue among patients with recurrent pterygium.
Citation: Liu J, Liu J, Xiong J, Yu Y, Yang X, et al. The Effect of Micro-Conjunctival Autografting Combined with Amniotic Membrane Transplantation on Treating Recurrent Pterygium: a Non-randomized Controlled Trial. J Clin Med Surgery. 2022; 2(2): 1058.
Introduction
Recurrent pterygium is a common postoperative complication of pterygium excision with a minimum incidence of 1.44% [1], leading to the aesthetic decline, eye surface discomfort, visual acuity impairment or limitation of eye movement [2]. At present, autologous conjunctival transplantation is regarded as the first choice in normal conditions [3]. However, for patients with recurrent pterygium undergone an transplantation, an extensive conjunctiva loss and a severe ocular surface damage may already exist. Moreover, the secondary acquisition of conjunctival flap undoubtedly aggravates the damage to the ocular surface environment. Furthermore, considering the high incidence of angle-closure glaucoma in middle-aged and elderly Asian people [4], routine conjunctival transplantation may take challenges for the possible trabeculectomy, such as the conjunctiva or cornea impairment related to the filtration bleb. For the prevalent dry eye [5], multiple conjunctival surgeries can increase the risk of postoperative dry eye. Though amniotic membrane transplantation is not the preferred surgical method for the treatment of recurrent pterygium, it can save the conjunctiva for pterygium excision [6,7].
Therefore, our research aimed to use micro-conjunctival transplantation (2.0 mm × 3.0 mm) to reconstruct limbal conjunctiva and amniotic membrane to cover the whole pterygium resection area to better protect conjunctival sac and ocular surface.
Methods
In this non-randomized Controlled Trial, patients with recurrent pterygium who received conventional conjunctival transplantation or micro-conjunctival autografting combined with amniotic membrane transplantation in the Second Affiliated Hospital of Nanchang University from March 2021 to May 2021 were involved. This study was approved by the ethics committee of the Second Affiliated Hospital of Nanchang University and followed the principles of Helsinki declaration. Informed consent was signed by all subjects. The study has been regis-The study has been registered on ClinicalTrials.gov (NCT05362253).
Participants
Inclusion criteria for the study were as follows: (1) age⩾18; (2) relapsed after pterygium surgery once; (3) invading the cor-relapsed after pterygium surgery once; (3) invading the cor-relapsed after pterygium surgery once; (3) invading the cor- nea 2.00~5.00 mm [8].
The exclusion criteria were: (1) having obvious severe systemic organic diseases and mental diseases; (2) In lactation or pregnancy or planned pregnancy; (3) combined with eye diseases such as severe eyelid insufficiency, dry eye, chemical injury of cornea and conjunctiva, etc.; (4) used drugs that may affect the growth and metabolism of corneal epithelium within four weeks before inclusion in the study [8-10]; (5) received pterygium surgery twice or more.
Data collection
The experimental group (n = 20, 21 eyes) received microconjunctival autograft combined with amniotic membrane transplantation while the control group (n = 20, 22 eyes) received given conventi onal autologous conjunctival transplanta-conventional autologous conjunctival transplanta-autologous conjunctival transplantation. Follow-up was done at 3 d, 7 d, 14 d, 1 m, 3 m and 6 m after operation. Visual acuity, intraocular pressure (IOP), pterygium size, ocular surface symptom scores, tear secretion assay, the repair of corneal epithelium and grade of conjunctival hyperplasia were performed and documented for all participants.
The pterygium size is recorded by the longest length of its invasion into the cornea. The ocular surface symptom scores include dryness, burning, foreign body and pain sensation. The full score of each symptom is 100 points, with a score of 0 reflecting no discomfort, 100 was considered as the maximum discomfort. The tear secretion assay adopted a 5-minute Schirmer test I. Corneal fluorescein sodium staining was applied to assess the epithelial repair after operation. The grade of conjunctival hyperplasia is divided into the following four grades: Grade 1, no significant difference from normal eyes (with no recurrence); Grade 2, a little episcleral vessels in the pterygium excision area, which extends to the corneoscleral limbus but does not exceed, and there is no fibrous tissue hyperplasia (no recurrence); Grade 3, having proliferative fibrous tissue in the resection area, which does not exceed the limbus (no recurrence); Grade 4, the cornea is invaded by proliferative fibrous tissue, and this grade is true pterygium recurrence (recurrence) [11]. Statistics shall be made according to each proliferation grade.
Surgical procedure
Conventional autologous conjunctival transplantation: Routine disinfection and anaesthesia. To bluntly separate and excise pterygium. Remove pterygium on the corneal surface with a round blade. Injecting 0.2 ml of 2% lidocaine under the superior temporal conjunctiva near the limbus, take the conjunctival epithelium equal to the size of the exposed scleral and translate it to the exposed scleral surface (the limbus side of the graft corresponds to the limbus of the graft bed). The conjunctival flap was anchored to the superficial scleral plane with a 10-0 suture. The free conjunctival margin of the conjunctival flap sampling area was sutured intermittently with 10-0 suture. Apply tobramycin dexamethasone eye ointment and wrap the eyes with dressing after operation.
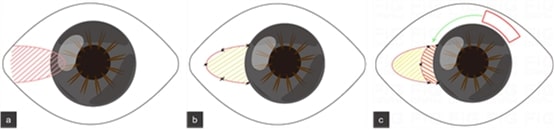
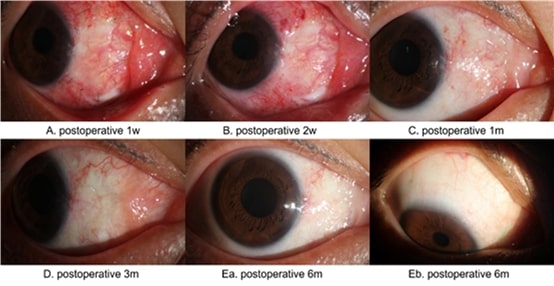
Micro-conjunctival autografting combined with amniotic membrane transplantation: Disinfection, anaesthesia and excision of recurrent pterygium are the same as conventional autologous conjunctival transplantation. The biological freeze-dried amniotic membrane (Jiangxi Ruiji Biological engineering technology Co., Ltd., Nanchang, China), equivalent in size to the exposed scleral surface, was flat mounted on the exposed scleral area (Figure 2C①+②), and fixed on the superficial sclera with 10-0 suture. 2% lidocaine was applied to the superior temporal conjunctiva. Take the conjunctival epithelial graft (Figure 2C③) with the length equivalent to the neck of recurrent pterygium and the width of 1.5 mm ~ 2.0 mm, and translate it on amniotic membrane surface near corneal limbus (Figure 2C②, the limbal side of the conjunctival epithelial graft corresponds to the limbal of the graft bed). The conjunctival flap was secured with 10-0 suture. Last, tobramycin and dexamethasone eye ointment was applied and bandaged with dressing. The surgical procedure is detailed in Figure 1. Preoperative and postoperative photographs of the anterior segment are shown in Figure 2A~2B.
Medication
The medication was consistent in all patients, the medication was consistent for all patients. Antibiotics were used locally 3 days before operation, antibiotics, glucocorticoids and repair promoting drugs were used locally one month after operation, and glucocorticoids were gradually reduced within one month.
Statistical analysis
The measurement data with normal distribution are expressed by "mean ± standard deviation (SD)", and the difference test was conducted by independent sample t-test. χ2 test was used to test the difference of counting data. The data of non- abnormal distribution were expressed by median (M) and range, and Mann-Whitney U test was used to test the significance of difference. Repeated measurement analysis of variance was used to evaluate visual acuity, IOP, Schirmer test and the scores of dryness, burning/acupuncture, foreign body and pain. P < 0.05 was regarded as statistically significant. SPSS 24. 0 was applied to perform statistical analyses.
Results
Baseline characteristics
The study included 43 eyes of 40 patients aged from 45 to 68 years with 3 patients dropped out (37 in group). There were no statistically significant differences in age, gender, visual acuity, intraocular pressure, pterygium size, Schirmer test I, dryness sensation, foreign body sensation, burning sensation, and pain sensation distribution between the two groups (Table 1).Table 1: General information and preoperative dates of the patients.
| Control group | Experimental group | P Value§ | |
|---|---|---|---|
| cases (eyes) | 20 (22) | 20 (21) | |
| Gender, male/female | 08-Dec | 09-Nov | 0.749 ‡ |
| Age (years) | 56.00 ± 7.17 | 57.95 ± 7.44 | 0.404 † |
| Eyesight, M(IQR) | 0.8 (0.5) | 0.8 (0.4) | 0.794 * |
| IOP (mmHg) | 14.73 ± 2.02 | 14.54 ± 2.10 | 0.759 † |
| Size of pterygium (mm) | 2.99 ± 0.73 | 3.29 ± 0.72 | 0.182 † |
| Schirmer test I(mm), M(IQR) | 11.25 (1.9) | 12.2 (3.2) | 0.568* |
| Dryness sensation | 13.82 ± 5.73 | 14.05 ± 4.58 | 0.886 † |
| burning sensation | 22.18 ± 7.14 | 23.29 ± 6.81 | 0.607 † |
| foreign body sensation | 22.77 ± 9.13 | 21.95 ± 8.35 | 0.760 † |
| Pain, M(IQR) | 3.00 (6) | 0.00 (6) | 0.717 * |
Data were presented as mean ± SD, No or M(IQR).
§ The P-value was for comparing the difference between Control group
and Experimental group.
† Independent two-sample t test. The normality was checked by Shapiro‒Wilk test.
‡ Chi-squared test
*Rank-sum test. The normality was checked by Shapiro‒Wilk test.
IOP: intraocular pressure, M: median, SD: standard deviation, IQR: interquartile range.
Postoperative recurrence
37 patients did not develop relapse within 6 months after operation, and there was no significant difference in the distribution of grade 1, 2 and 3 conjunctival hyperplasia between the two groups (P = 1.000>0.05) (Table 2). The photos of the anterior segment of the patients in the experimental group during postoperative follow-up are shown in Figure 3A~Eb.
Table 2: Comparison in corneal epithelial repair and grade of conjunctival hyperplasia.
| Group | Median | Minimum | Maximum | P§ | |
|---|---|---|---|---|---|
| Grade of conjunctival hyperplasia | Control group | 2 | 1 | 3 | 1.000* |
| Experimental group | 2 | 1 | 3 | ||
| Corneal epithelial repair time | Control group | 4 | 3 | 5 | 0.865* |
| Experimental group | 4 | 3 | 5 |
Data were presented as media, minimum and maximum.
§ The P-value was for comparing the difference between Control group and Experimental group.
*Rank-sum test. The normality was checked by Shapiro‒Wilk test.
Situation of corneal epithelial repair
The corneal epithelium healed between 3 and 5 d postoperatively in both groups, with no statistically significant difference between groups (P = 0.865 > 0.05) (Table 2).
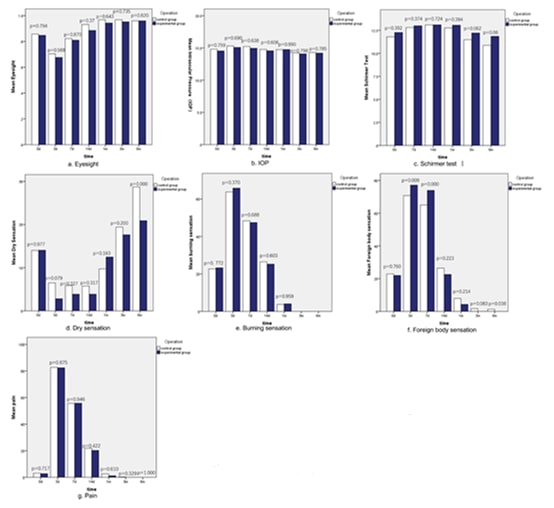
Evaluation of dry eye
At 6 months after operation, the dryness score of the control group was significantly higher than that of the experimental group (P = 0.000 < 0.05), and there was no significant difference between the two groups at other time points. The foreign body sensation score of the experimental group was higher than that of the control group at 3 days (P = 0.009 < 0.05) and 7 days (P = 0.000 < 0.05) after operation, and there was no significant difference between the two groups after suture removal (14 d, 1 m, 3 m and 6 m after operation). Schirmer test I there was no statistical significance in the differential analysis between groups at all-time points after operation, but as can be seen by fig 4 c that the result of Schirmer test I in the control group showed a greater downward trend than that in the experimental group after postoperative 14 days. There was no significant difference in visual acuity, IOP, burning sensation and pain between the two groups at each time point after operation (Figure 4a~4g).
Limitations
Complications
During the 6-month follow-up period, no complications such as graft inversion and necrosis, haemorrhage, granulomas, scleral lysis, donor site conjunctival scarring, and steroid-induced ocular hypertension were found in this study.
Discussion
Our study proved that micro-conjunctival autograft combined with amniotic membrane transplantation protecting the ocular surface while reducing the risk of postoperative dry eye by greatly saved the conjunctiva. Moreover, this operation can reserve more conjunctiva for potential glaucoma patients to form filtering blebs during trabeculectomy.
Recurrent pterygium occurs mostly in middle-aged and elderly people [12]. Hence, the preious conjunctival autograft, the past or potential trabeculectomy for angle closure glaucoma, dry eye, and some other ocular diseases bring challenges for the pterygium surgery. The reducing available conjunctiva and the impaired ocular surface make a large conjunctival flap graft difficult, bringing need for other covering materials. Amniotic membranes are widely used in various ocular surface diseases [13], providing an extracellular matrix for the exposed sclera in pterygium. Therefore, our study attempts to use smaller conjunctival flap combined with amniotic membrane to treat recurrent pterygium, integrate their advantages and make up for each other's shortcomings, which not only reduces the requirements for patients' conjunctival conditions, but also ensures a low recurrence rate.
For recurrent pterygium after autologous conjunctival transplantation, most of the recurrence of pterygium occurred within the first 3 or 6 months after surgery.[14] Therefore, 3 and 6 months after operation are important time points to observe the recurrence of pterygium. This study showed that there was no true recurrence of pterygium within 6 months, which was consistent with the existing research results [15,16]. Previous research showed optimistic recurrence of sutureless amniotic membrane transplantation combined with narrow-strip conjunctival autograft in primary pterygium [17]. In our study, micro-conjunctival autograft combined with amniotic membrane transplantation showed lower recurrence than that of amniotic membrane transplantation reported in the literature,[18] and also significantly lower than that of amniotic membrane transplantation combined with autologous conjunctival transplantation reported in the past [19]. The possible reasons may be as follow: (1) The exposed sclera after pterygium excision was completely covered by the amnion membrane for conjunctival epithelium growth, while the limbal barrier was reconstructed by micro-conjunctival graft covered the limbal side of amniotic membrane graft. (2) The postoperative use of glucocorticoids can effectively inhibit the inflammation. (3) The operative durations were reduced by the skilled surgeon.
The recurrent pterygium related dry eye were also assessed [20], while the tear breakup time (TBUT) was not included for the influence of postoperative corneal epithelial defect. The foreign body sensation score of the experimental group was higher than that of the control group before suture removal, but no significant difference in foreign body sensation score between the two groups after suture removal, which may be related to the more and scattered sutures of micro-conjunctival autograft combined with amniotic membrane transplantation. The dryness sensation scores of patients in the control group were higher than those in the experimental group at 6 months after operation, and Schirmer test I results showed a larger decreasing trend than that in the experimental group after post-operative 14 days, which may be related to the larger size of the conjunctival flap retrieved intraoperatively in the control group than in the experimental group. No statistically significant differences were found in burning sensation, pain, corneal epithelial repair time, visual acuity, and IOP between the two groups. To sum up, the long-term results of the ocular symptom scores in the experimental group were better than those in the control group. This is similar to the research results of Yu Jing et al [8].
Limitations
There are still some limitations in this study. First, the symptom scores on the ocular surface are related to the discomfort tolerance of each patient with strong subjectivity, and there may be some deviations in the results. These biases can be reduced by paying long-term attention to patients' symptom scores and their change curves. Second, a longer follow-up and a large sample size are still needed to obtain the long-term effect of micro-conjunctival autograft combined with amniotic membrane transplantation in the treatment of recurrent pterygium.
Conclusion
In conclusion, the study showed a small conjunctival graft, little disturbance on the ocular surface microenvironment, and a lower recurrence rate in micro-conjugation autograft combined with amniotic membrane transplantation, which can provide a safe surgical modality for the treatment of recurrent pterygium in Asian population with more complex anterior segment conditions.
Declarations
Competing interests: one declared.
Funding: This research was supported by the Major project of Natural Science Foundation of Jiangxi Province (20212ACB206022), the Traditional Chinese Medicine Scientific Research Fund Project of Jiangxi Province (2019A1889), and the Science and Technology Foundation of Jiangxi Provincial Health Commission (202110043 and 202310521).
Acknowledgements: The authors thank the Figdraw of Home for Researchers platform for its support for image production. Figure 1 and Figure 2C is done on the Figdraw of Home for Researchers platform (the export ID: WAUIA71fa1, IOUYUd558b, PUIRAae48d, YOUI7471d).
Ethics approval: Ethics approval was obtained from the ethical review committee of The Second Affiliated Hospital of Nanchang University.
Data availability statement: Data are available on request. Any requests for data can be made to the corresponding author and are subject to ethics approval.
References
- Kodavoor SK, Preethi V, Dandapani R. Profile of complications in pterygium surgery - A retrospective analysis. Indian J Ophthalmol. 2021; 69: 1697-1701.
- Farid M, Lee N. Ocular surface reconstruction with keratolimbal allograft for the treatment of severe or recurrent symblepharon. Cornea. 2015; 34: 632-636.
- Nava-Castañeda A, Ulloa-Orozco I, Garnica-Hayashi L,HernandezOrgaz J, Jimenez-Martinez MC, et al. Triple subconjunctival bevacizumab injection for early corneal recurrent pterygium: one-year follow-up. J Ocul Pharmacol Ther. 2015; 31: 106-113.
- Bikbov MM, Gilmanshin TR, Zainullin RM, Kazakbaeva GM, Arslangareeva II, et al. Prevalence and associated factors of glaucoma in the Russian Ural Eye and Medical Study. Sci Rep. 2020; 10: 20307.
- Kawashima M, Tsubota K. Effect of calorie restriction on change in lacrimal gland with age. Cornea. 2011; 30: S29-33.
- Shusko A, Hovanesian JA, Pterygium excision with conjunctival autograft and subconjunctival amniotic membrane as antirecurrence agents. Can J Ophthalmol. 2016; 51: 412-416.
- Rosen R. Amniotic Membrane Grafts to Reduce Pterygium Recurrence. Cornea. 2018; 37: 189-193.
- Yu J, Feng J, Jin T, Tian L, Zhu L et al. The Effect of a Novel Strategy in Treating Primary Pterygium: A Prospective Randomized Clinical Study. Am J Ophthalmol. 2021; 225: 108-116.
- Sul S, orkmaz S, Alacamli G, Ozyol P, Ozyol E, et al. Application of autologous serum eye drops after pterygium surgery: a prospective study. Graefes Arch Clin Exp Ophthalmol. 2018; 256: 1939- 1943.
- Kampitak K, Leelawongtawun W, Leeamornsiri S, Suphachearaphan W, et al. Role of artificial tears in reducing the recurrence of pterygium after surgery: a prospective randomized controlled trial. Acta Ophthalmol. 2017; 95: e227-e229.
- Prabhasawat P, Barton K, Burkett G, Tseng SC. Comparison of conjunctival autografts, amniotic membrane grafts, and primary closure for pterygium excision. Ophthalmology. 1997; 104: 974-985.
- Vinker S, Segal O, Mimouni M, Kaiserman I, et al. Epidemiology and Associated Morbidity of Pterygium: A Large, Community-Based Case-Control Study. Semin Ophthalmol. 2016; 31: 446- 451.
- Hino T, Sotozono C, Inatomi T, Fukuoka H, Nakamura T, et al. Indications and surgical outcomes of amniotic membrane transplantation. Nippon Ganka Gakkai Zasshi. 2012; 116: 374-388.
- Ti SE, Chee SP, Dear KB, Tan DT. Analysis of variation in success rates in conjunctival autografting for primary and recurrent pterygium. Br J Ophthalmol. 2000; 84: 385-389.
- Barbosa JB, Costa De Farias C, Hirai FE, Pereira Gomes JA, et al. Amniotic membrane transplantation with narrow-strip conjunctival autograft vs conjunctival autograft for recurrent pterygia. Eur J Ophthalmol, 2017; 27: 135-140.
- Dupps WJ, Jr, Jeng BH, Meisler DM. Narrow-strip conjunctival autograft for treatment of pterygium. Ophthalmology. 2007; 114: 227-231.
- Taylan Sekeroglu H, Erdem E, Dogan NC, Yagmur M, Ersoz R, et al. Sutureless amniotic membrane transplantation combined with narrow-strip conjunctival autograft for pterygium. Int Ophthalmol. 2011; 31: 433-438.
- Röck T, Bramkamp M, Bartz-Schmidt KU, Röck D et al. A Retrospective Study to Compare the Recurrence Rate After Treatment of Pterygium by Conjunctival Autograft, Primary Closure, and Amniotic Membrane Transplantation. Med Sci Monit. 2019; 25: 7976-7981.
- Kenyon KR, Wagoner MD, Hettinger ME. Conjunctival autograft transplantation for advanced and recurrent pterygium. Ophthalmology. 1985; 92: 1461-1470.