Clinical & Medical Surgery
Open Access
Volume 2
Xiang Zhang1; Man-ying Lin2ⴕ; Xi-wen Feng1ⴕ; Jia-jun Wu1; Wei Cai1; Bin-jun Tong1; Mian-zhi Chen1; Bang-sheng Cui1*
*Corresponding Author: Bang-sheng Cui
TGuangzhou University of Traditional Chinese Medicine ShunDe Traditional Chinese Medicine Hospital, China.
Email: zhangxiang621@163.com
Article Info
Received: Oct 08, 2022
Accepted: Oct 31, 2022
Published: Nov 07, 2022
Archived: www.jclinmedsurgery.com
Copyright: © Bang-sheng C (2022).
Abstract...
Background: Venous ulcer is an open skin lesion that is difficult to heal and easy to recur. Although the fatality rate is low, the quality of life of patients is seriously affected, and there is the possibility of infection, deterioration and even amputation. The use of platelet rich plasma therapy has obvious effect, but the combined treatment of great saphenous vein dissection is rarely reported.
Methods: The present case report is 59-year-old male patient who has had venous leg ulcer, measuring 8 × 4 cm and about 0.5 cm deep. He was hospitalized several times for symptomatic treatment but failed to recover after conventional wound treatment. The patient was transferred to our wound treatment team, and after PRP combined with saphenous vein dissection, the venous ulcer healed completely.
Clinical discussion: Venous ulcer can change patient’s quality of life and lead to infection and amputation. Thus, efficient therapeutic methods are necessary for management of venous ulcer.
Conclusion: PRP combined with saphenous vein dissection not only could significantly improve the wound healing effect, shorten the wound healing time, but also reduce the itching, pain and recurrence rate, and improve their quality of life. Therefore, it is recommended that wound care teams use this approach to speed up the healing process.
Citation: Zhang X, Man-ying L, Xi-wen F, Jia-jun W, Bang-sheng C, et al. Reviving Hope by Using Platelet-Rich Plasma Combined with Saphenous Vein Stripping Surgery in Patients with Refractory Venous Leg Ulcer: A Case Report. J Clin Med Surgery. 2022; 2(2): 1056.
Introduction
Venous Leg Ulcer (VLU) is a group of open skin lesion due to varicose vein disease. The common reason is increased venous dynamic pressure caused by venous wall and valve insufficiency. VLU accounts for about 70% of all lower extremity ulcers, often occurring in the boot area, with the characteristics of difficult to heal, long course of disease and easy to relapse [1]. Pathogenesis of VLU is continuous venous hypertension of lower limbs caused by venous insufficiency or obstruction, which could leads to local blood circulation and tissue absorption disorders, accumulation of metabolites, tissue malnutrition, lower limb edema and skin nutritional changes [2]. Although the fatality rate of VLU is low, it seriously affects the quality of life, and it may lead to infection, deterioration or even amputation. Studies have shown that 60% of patients’ ulcer surface healed within 3 to 6 months, 33% healed within 1 year, and 7% may be refractory for life. In addition, the recurrence rate of patients after ulcer surface healing 3-5 months can be as high as 70% [3]. The incidence of ulcer for more than 10 years of chronic venous insufficiency is 10% [4], and the recurrence rate of ulcer is up to 70% without corresponding nursing measures after surgical treatment [5].According to the survey, the incidence of VLU in Britain and Sweden is 0.2-0.5%, and that in China is about 0.4-1.3%, with the increasing incidence year by year [6].
Open surgery is the traditional method for the treatment of VLU, which mainly includes high vein ligation, saphenous vein stripping surgery and ligation of traffic veins. At present, minimally invasive treatment, such as radiofrequency ablation, ultrasound guided foam sclerotherapy injection therapy has been promoted in clinical practice. On the other hand, patients with refractory VLU may have a concurrent iliac vein or vena cava system compression syndrome. Intravenous stenting could improve venous return, reduce limb edema, and relieve pain, but there is no evidence to prove that it can reduce ulcer symptoms or prevent recurrence [7]. Compression can reduce venous reflux and venous edema, promote oxygenation of skin tissue around ulcer, and ultimately stimulate fibrinolysis. Therefore, compression therapy is the basic treatment for VLU [1]. However, due to the relative contraindications of treatment such as heart failure and lower limb arteriosclerosis occlusion. In addition, the more serious problem is that the ulcer wound still persists after treatment. Therefore, the local treatment of VLU wound is equally important.
Platelet-Rich Plasma (PRP) is plasma with high concentration of platelets separated from the whole blood by centrifugation. It secretes a variety of substances that enhance the natural healing process of the injured area. After applied to the wound, PRP can activate platelets and release a large number of growth factors and cytokines with high concentration [8], including platelet-derived growth factor (PDGF), transforming growth factor β1(TGF-β1), transforming growth factor β2(TGF-β2), Insulin-Like Growth Factor (IGF), epidermal growth factor (EGF), vascular endothelial cell growth factor (VEGF) [8]. It further promotes cell division and proliferation, induce the synthesis of extracellular matrix and bone matrix, which can play an auxiliary role in local granulation tissue growth. At the same time, PRP contains high concentration of white blood cells, which could kill pathogenic microorganisms on the surface of the wound by chemotaxis and phagocytosis, thus playing a certain antibacterial role [9]. Compared with antibiotics, PRP do not induce antibiotic resistance. Moreover, it has a good synergistic effect on preventing wound infection by disease-resistant microorganisms and promoting wound healing [10].
The characteristics of high incidence, recurrence and long treatment period of VLU result in the limitation of patients’ personal activities and increased social psychological pressure. Multiple surgical treatment will inevitably lead to increased medical costs. PRP is effective in the treatment of refractory ulcers, but there are few reports on PRP combined with saphenous vein stripping surgery. Therefore, this study analyzed and reviewed a patient with refractory VLU who healed quickly after treatment with PRP combined with saphenous vein stripping surgery, and no recurrence was observed during a 4-year follow-up.
Case presentation
This case is a 59-year-old male patient with venous ulcer from Foshan, China. He lived in a low socioeconomic family and had only a primary school education. He was working in a processing factory and had a sedentary lifestyle. In May 2016, he first experienced swelling in his left lower limb, which gradually spread to the left medial calf near the ankle, accompanied with skin itching, pigmentation, skin lesions. He ignored it and developed a left leg ulcer with effusion 3 weeks later. Then he was treated at a local hospital with Epidermal Growth Factor (EGF) biologics to promote wound healing, but the symptoms continued to recur. His condition continued to deteriorate by the end of 2017, so he came to our hospital in May 2018. The patient denies any other chronic history or infectious disease and his family history was unremarkable.
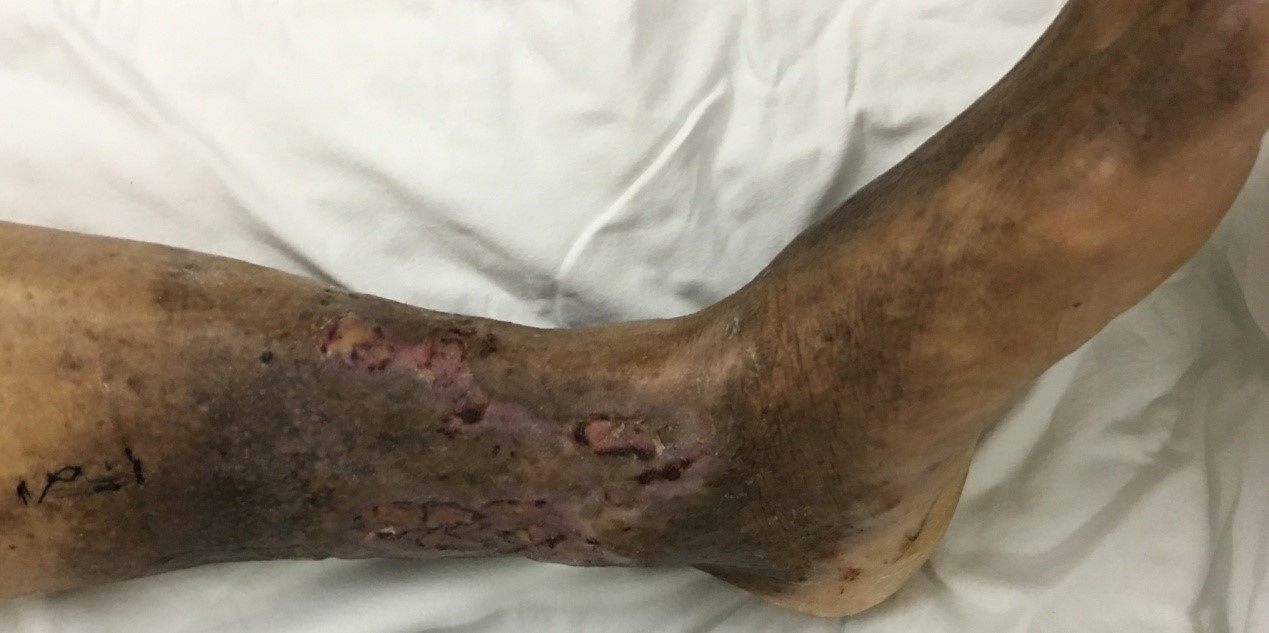
During history-taking and physical assessment this condition resulted in the formation of a VLU on the medial side of the left calf near the ankle, measuring 8 × 4cm and about 0.5cm deep (Figure 1). The surface of the ulcer is dark red and covered with dirty gray rot and smelly pus.
The vital signs of patient on admission were as follows: Pulse Rate: 80 Beat Per Minute (BPM); Temperature: 37°C; Blood Pressure: 120/80 mmHg; Respiration Rate: 12 bpm. The complete blood count (CBC) shows an elevated white blood cell count and low lymphocyte, hemoglobin, and platelet counts. Biochemical test indicated abnormal liver and kidney function. Screening for metabolic and systemic autoimmune diseases revealed rheumatoid factor: (+), accompanied by elevated detection of hypersensitive C-reactive protein hsCRP and anti-cyclocitrullinate peptide antibodies (Anti-CCP-Ig). Gram staining showed G+ cocci: (+); Gram stain G- bacillus: (+). General bacterial culture: there are 2 kinds of G+ coccus and 1 kind of G+ bacillus. The other test results were not significant.Some laboratory data of the patient during admission are provided as follows (Table 1).
First, we obtain written informed consent from the patient and sign written consent for surgery and related treatment. Then we preoperative continuous cleaned wound (Figure 2) and adjust his liver and kidney function. Due to the patient’s persistent wound and bacterial culture (+), the surgery was performed in stages. Wound debridement and saphenous vein extraction were performed in the first operation. The operation was completed in accordance with the prescribed procedure (Figure 3). We postoperative cleaned wound, coordinated to change dressing, and the patient’s condition has been closely observed. Five days later, dermatoplasty and PRP infusion were performed in the operating room, and the operation was completed in accordance with the prescribed procedure (Figures 4,5). These surgeries are performed by professional orthopedic surgeons. Therasorb(R) Algiplus Adhesive Dissing (AD) gel excipients were used to cover the patient’s wounds for 1 week. One week later, no necrotic tissue was found on the wound surface, but granulation tissue appeared (Figure 6). Two weeks after surgery, the wound healed well and the skin graft area survived (Figure 7). During discharge, the patient was advised to avoid excessive weight bearing on the left lower limb and to keep the wound area free of compression. Reexamination 3 months after the operation showed that the wound had healed completely (Figure 8). During discharging stage, the patient was educated to prevent putting excessive pressure on the area and uses a crutch or wheelchair.
Table 1: The patient’s laboratory information during admission.
| Cell blood count (CBC) | Biochemistry |
|---|---|
| WBC: 12.40 × 109/L | CREA: 117.60 μmol/L |
| HGB: 128 g/L | GLU: 6.58 μmol/L |
| PLT: 101 × 109/L | ALP: 153.00 U/L |
| ESR: 6.00 mm/h | AST: 50.90 U/L |
| RF: 137 IU/ml | ALT: 87.90 U/L |
| hsCRP: 10.60 mg/l | GGT: 564.00 IU/L |
| Anti-CCP-Ig: 46.08 U/ml | Coagulation Function |
| CRP: 17 mg/L | D-D: 0.77 μg/ml |
| General bacterial smear test | APTT: 22.90 sec |
| Gram-positive cocci: + | General bacterial culture |
| Gram-negative bacillus: + | Staphylococcus aureus |
Discussion
Although many studies have revealed the mechanisms of injury, inflammation and repair of VLU, the specific pathogenesis remains unclear. After the theory of white blood cell capture was put forward, the research on white blood cell and related factors was deepened. Some studies have proved that it is correlated with adhesion molecules, chemotactic cytokines and oxidative stress response, leading to systemic imbalance between inflammatory mediators and anti-inflammatory factors [11]. The long-term imbalance between inflammatory mediators and anti-inflammatory factors in VLU could induce canceration of ulcers. Serious complications include infections and skin cancers such as squamous cell carcinoma [1]. Therefore, based on the characteristics and complications of VLU, early diagnosis and treatment is particularly important.
This case emphasizes the success of PRP combined with saphenous vein dissection in the treatment of refractory venous stasis ulcer. The operation of saphenous vein has a long history. Since modern times, Trendelenburg, Keller and other scholars [12] have proposed the surgical method for the treatment of diseased vein. Nowadays, saphenous vein stripping and perforating vein dissection have become the standard surgical procedures, including high saphenous vein ligation, branch fragmen- tation, trunk stripping, perforating vein ligation, and varicose vein punctate stripping, etc. Superficial vein surgery not only can reduce the recurrence rate of ulcer, but also improve the cure rate of refractory VLU to a certain extent compared with conservative treatment [13]. PRP is a new treatment method for ulcer wounds in recent years. It mainly extracts the patient's own venous blood, obtains platelet-rich plasma through centrifugation and concentration, then adds gel-like substances to make gel and smear it on the wound surface. They can be classified into Autologous Platelet-Rich Plasma (AU-PRP) and Allogeneic Platelet-Rich Plasma (AL-PRP) [14]. AU-PRP does not cause immune rejection due to its origin in the patient. Therefore, PRP is generally referred to as AU-PRP in clinical practice and it is usually applied to wound repair in the form of Autologous Platelet-Rich Gel (APG). The level of platelets in PRP is 3-5 times higher than in venous blood [15], and it can release a variety of growth factors after activation [9], thus promoting the regeneration of ulcer surface tissues and blood vessels. It is activated by thrombin and calcium to form a gel, and the large amount of fibrin in the gel acts as a biological scaffold, which can induce effective healing of ulcer surface. In addition, PRP can inhibit pseudomonas aeruginosa and other bacteria [16]. As we know, PRP was originally used for the treatment of thrombocytopenia. Due to its unique biological effect, PRP has great advantages in promoting wound healing, skin rejuvenation and sports injury repair, etc. It has been widely used in wound repair, plastic surgery and orthopedics [17].
The treatment of VLU is not a simple procedure, and it is still a difficult problem for patients and doctors. The occurrence, development and prognosis of VLU are determined by several factors. Usually, the precursor of successful treatment is the comprehensive treatment concept with surgery as the main, conservative treatment as the auxiliary, and with multifaceted integration. It requires the orthopedic surgeon to have a comprehensive understanding of its pathogenesis and the origin of multiple treatment methods. The precision of venous positioning and visualization of manual operation have been realized with the progress of modern science and technology. Unfortunately, current clinical attention is generally paid to the healing or recurrence of ulcerous surface, while the continuous management of ulcerous surface is neglected. This includes public education such as living habits, weight control, scientific exercise and awareness training. At the same time, case-control studies based on large samples and long-term follow-up data on clinical outcomes are still scarce. Various treatment guidelines need to be harmonized. In addition, recommendations for increased pain management and compliance, especially in older patients, are also urgently needed.
Conclusion
In conclusion, we treated one patient with refractory VLU by autologous PRP combined with saphenous vein surgery, and there was no recurrence in 4 years follow-up. This case indicates that this method is effective in treating refractory VLU. It not only could significantly improve the wound healing effect, shorten the wound healing time, but also reduce the itching, pain and recurrence rate, and improve their quality of life. Therefore, it is recommended that wound care teams use this approach to speed up the healing process.
Declarations
Conflicts of interest: the author declares that there is no conflict of interest.
Ethical approval: This study was approved by the Shunde Hospital GuangZhou University of Chinese Medicine (KY- 2019030).
Informed consent: All included patients or their deputies provided written informed consent.
Abbreviations: VLU: Venous Leg Ulcer; PRP: Platelet-Rich Plasma; PDGF: Platelet-Derived Growth Factor; TGF-β1: Transforming Growth Factor Β1; TGF-β2: Transforming Growth Factor Β2; IGF: Insulin-Like Growth Factor; EGF: Epidermal Growth Factor; VEGF: Vascular Endothelial Cell Growth Factor; EGF: Epidermal Growth Factor; BPM: Beat Per Minute; CBC: Complete Blood Count; hsCRP: Hypersensitive C-Reactive Protein; Anti-CCP-Ig: Anti-Cyclocitrullinate Peptide Antibodies; AU-PRP: Autologous Platelet-Rich Plasma; AL-PRP: Allogeneic Platelet-Rich Plasma; APG: Autologous Platelet-Rich Gel
References
- Alavi A, Sibbald RG, Philips TJ, Miller OF, Margolis DJ, et al. What’s new: Management of venous leg ulcers Treating venous leg ulcers. J Am Acad Dermatol. 2016; 74: 643-666.
- Crawford JM, Lal BK, Durán WN, Pappas PJ. Pathophysiology of venous ulceration. J Vasc Surg Venous Lymphat Disord. 2017; 5: 596-605.
- Finlayson K, Wu ML, Edwards HE. Identifying risk factors and protective factors for venous leg ulcer recur rence using a theoretical approach: a longitudinal study. Int J Nurs Stud. 2015; 52: 1042-1051.
- Bonkemeyer Millan S, Gan R, Townsend PE. Venous ulcers: diagnosis and treatment. Am Fam Physician, 2019; 5: 298-305.
- Abelyan G, Abrahamyan L, Yenokyan G. A case-control study of risk factors of chronic venous ulceration inpatients with varicose veins. Phlebology. 2018; 33: 60-67.
- Sun Y, Yuan B, Li CM. Research progress of compression therapy in the prevention of lower limb deep vein thrombosis. Chin J Gen Pract. 2020; 19: 145-149.
- Raju S, Owen Jr S, Neglen P. The clinical impact of iliac venous stents in the management of chronic venous insufficiency. J Vasc Surg. 2002; 35: 8-15.
- Jee CH, Eom NY, Jang HM, Jung HW, Choi ES, et al. Effect of autologous platelet-rich plasma application on cutaneous wound healing in dogs. J Vet Sci. 2016; 17: 79-87.
- Pereira RCDF, Desessards DLCF, Brass KE, da Silva Azevedo M, Gallio M, et al. Evaluation of Three Methods of Platelet-Rich Plasma for Treatment of Equine Distal Limb Skin Wounds. J Equine Vet Sci. 2019; 72: 1-7.
- Fernando DLP, Muñoz-Cruzado MVD, Maestre MV, García-Ca-brera AM, Luisa Reyes M et al. Plateletrich plasma (PRP) versus fibrin glue in cryptogenic fistula-in-ano: a phase III single-center, randomized double-blind trial. Int J Colorectal Dis. 2019; 34: 1113-1119.
- Sirbi AG, Florea M, Patrascu V, Rotaru M, Gabriel Mogoş D, et al. Squamous cell carcinoma developed on chronic venous leg ulcer. Rom J Morphol Embryol. 2015; 56: 309-313.
- Bonkemeyer Millan S, Gan R, Townsend PE. Venous ulcers: Diagnosis and treatment. Am Fam Physician. 2019; 100: 298-305.
- Thomas CA, Holdstock JM, Harrison CC, et al. Healing rates following venous surgery for chronic venous leg ulcers in an independent specialist vein unit. Phlebology. 2013; 28: 132-139.
- Pachito DV, Latorraca C, Riera R. Efficacy of platelet-rich plasma for non-transfusion use: Overview of systematic reviews. Int J Clin Pract. 2019; 73: e13402.
- Everts P, Onishi K, Jayaram P, Lana JF, Mautner K, et al. Platelet-Rich Plasma: New Performance Understandings and Therapeutic Considerations in 2020. Int J Mol Sci. 2020; 21.
- Cetinkaya RA, Yenilmez E, Petrone P, Yılmaz S, Bektöre B, et al. Platelet-rich plasma as an additional therapeutic option for infected wounds with multi-drug resistant bacteria: in vitro antibacterial activity study. Eur J Trauma Emerg Surg. 2018; 45: 555- 565.
- Alves R, Grimalt R. A Review of Platelet-Rich Plasma: History, Biology, Mechanism ofAction, and Classification. Skin Appendage Disord. 2018; 4: 18-24.