Clinical & Medical Surgery
Open Access
Volume 2
Alessandro Crisci1,2,3*; Michela Crisci4
*Corresponding Author: Alessandro Crisci
Department of Medicine, Surgery and Dentistry, Salernitan Medical School, University of Salerno, Fisciano (SA), Italy.
Tel: +039 3388722799; Email: alessandrocrisci@libero.it
Article Info
Received: Oct 06, 2022
Accepted: Oct 28, 2022
Published: Nov 04, 2022
Archived: www.jclinmedsurgery.com
Copyright: © Crisci A (2022).
Abstract...
The surgical techniques used to close a primary wound, while sharing common principles and suture material, are multiple. With guaranteed aseptic wound conditions, modern requirements focus on achieving optimal aesthetic results. We present a V-Y suture technique that allows you to obtain a low tension suture, levelled with adaptation to the dermo-epidermal interface of the wound. Our technique is particularly suitable for indications in cosmetic plastic surgery, where high distracting forces of the wound in the transition phase between the aesthetic subunits typically occur with the cancer removal of the face in particular of the neck. The designed technique has never been applied to date.
A 92-year-old Caucasian female underwent excision for invasive basal cell carcinoma of 5 x 3 cm, located in the left lateral part of the neck. The operative deficiency has been repaired with a horizontally modified flap V-Y advancement peduncle. No postoperative complications occurred. Aesthetics result was optimal, without functional disturbances.
The peduncular advancement flap V-Y is one of the few procedures used to close localized surgical defects. Technical execution must be careful and requires adequate anatomical knowledge, since only in this way will it be possible to obtain acceptable aesthetic and functional results.
In conclusion, the modified V-Y flap (V-T flap) of which the technique is described guarantees an undistorted flap that can slide to the maximum possible position by aligning the margins of the epidermal zone wound directly adjacent to each other with consequently favorable forces of vector distribution of tension along the wound margins.
Citation: Crisci A, Crisci M. Rethinking a Reconstructive Technique: A Modified V-Y Flap Suture Technique with Horizontal Branch. Presentation of a Clinical Case. J Clin Med Surgery. 2022; 2(2): 1055.
Introduction
Several surgical suture techniques for both primary and secondary injury repair have been handed down through generations of surgeons, often before the “aseptic era” with sterile field surgery or scientific literature. Therefore, standard suture techniques are commonly, and in the authors’ perception somewhat vague, elaborated within books. Here, clinical outcomes are essentially considered as a consequence of individual surgery or patient-specific risk factors, such as diabetes. Recent publications mainly focus on the comparison of “standard techniques” for various outcome parameters [1]. We, therefore, see a certain need for further attention on how to execute a new V-Y flap in a reproducible manner. This requires a critical assessment and a concise, step-by-step description of the technique. However, to achieve both smooth wound healing and an aesthetically pleasing scar, this suture must:
(i) seamlessly connect wound edges [2],
(ii) minimizing the distraction of the tensile force vectors to the epithelial-dermal interface, avoiding
(iii) impair blood supply to the skin [3].
We present in detail a modified V-Y flap suture technique with a horizontal branch with the basic rationale of obtaining
(i) seamless, low-voltage wound adaptation on the wound surface,
(ii) adapting a maximum of the corresponding dermal and subcutaneous surfaces of the wound together with a limited load on the suture material and
(iii) an aesthetic result that is as acceptable as possible
This method of stitching is particularly suitable for indications in plastic surgery where high tensile forces can typically occur in areas of transition between the exposed aesthetic subunits (face, neck, etc.), and where the best possible outcome of the scar is fundamental.
Compared to skin grafts and free flaps, the local flap is advantageous because less scar tissue forms after reconstruction and the use of similar adjacent tissue offers aesthetic advantages and does not present the risk of donor site morbidity. Therefore, primary scarring and local patch are often used, although primary closure is more advantageous than local flap because it is a simpler surgical method and the scar has a linear shape. However, a wedge incision is required for circular soft tissue defects and, therefore, it is inevitable to sacrifice normal tissue. In addition, since the scar is often extensive, primary suturing is inconvenient because of the excessive tension that is inflicted on areas where the amount of skin tissue is inadequate.
Given the assumption described above, to minimize the sacrifice of normal tissue and avoid complications such as dog ears or excessive tension, we used a unilateral VY advancement flap to restoring soft tissue deficits later surgical excision of a head skin tumor [4-6].
Case presentation
The correct planning and implementation of the VY flap is, of course, fundamental to obtaining reproducible aesthetic results with the minimum operative risk [7,8].
This procedure has conducted on a patient about 92 years old female, non-smoker, chronic bronchopathic, F.C. 97 b/min, p.a. 140/80 mmHg.
On blood count: WBC 10.2 K/L (range: 4-11); RBC 4.22 M/L (range: 3.8-5.8); Hb 8.6 g/dL (range: 11.5-16.5); MCV 69 fL (range: 76-96); MCH 20.3 Pg (range: 27-32); MCHC 29.6 g/dL (range: 30-36).
To obtain written consent, all the appropriate hospital rules and regulations were followed by the patient in relation to the presented exemplary case, before taking photos and/or videos with the intention of publishing this technique. To minimize recurrences, we normally perform extensive removal. In addition, we use a 3 to 5 mm free margin in the case of basal cell carcinoma, 1 cm in the case of squamous cell carcinoma and 2.5 cm in the case of malignant melanoma [9,10].
As for single points (loops), three standard knotting techniques, performed manually or with a needle holder are commonly used: (1) square knot, (2) surgeon knot (syn.: knot friction) and (3) pivot knot.
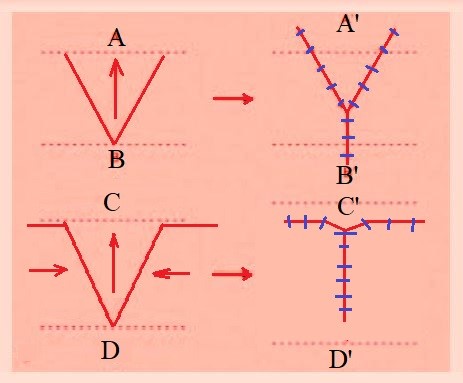
This method we adopted, in this case, involves transferring a classic V-flap to the site of the defect and converting it to a Y-flap using a random pattern flap involving the dermal plexus and the subcutaneous plexus, which are connected by a subcutaneous perforating artery derived from the muscle [5] (Figure 1 A, B).
The flap tested by the Authors and reported, given the conformation and site of the lesion, is a modified V-Y flap with a horizontal branch and, although it is categorically a skin flap with a random pattern, this VY flap has a more abundant and predictable blood flow than that of many other alternative reconstructive options. This improved vascular support can be beneficial in patients with an increased risk of tissue ischemia (smokers, patients with previous exposure to radiation therapy, the elderly, etc.).
On histopathological examination: cutaneous lozenge of 1.7 × 0.8 × 0.2 cm, centered by the detected dyschromic lesion. Histologically, after inclusion in paraffin and staining with hematoxylin-eosin, Basal cell carcinoma with nodular pattern was found. Free lateral surgical margins (>1 mm).
The modified V-Y feed flap is particularly useful when a structure or region requires elongation or release from a contracted state. It provides (Figure 1 C, D) to sculpt not only the central V as in the conventional V-Y flap (drawing A-B), but also a horizontal branch superior to the V that cleaves the neoplasm. The closure of the classic V-Y flap is Y-shaped, while that of the modified flap is much less Y-shaped, almost T-shaped, so we would call it the V-T flap. When this flap is used, less scar tissue is formed, which leads to less deformity of the seat, compared to when the conventional V-Y flap is used. Therefore, using the horizontal branch feed flap VY we obtained an excellent aesthetic result in the facial region (Figure 2D).
The enlargement of a scar is linked to ongoing tension [11].
Based on geometrical investigation, concerning a pivot flap including a flap of rotation and a transpositional flap, the modified V-Y feed flap results in less tension, which decreases the risk of hypertrophic alterations and long-term scar enlargement. On the other part, the V-Y patch has a lower degree of displacement; therefore, due to lower tension, it causes fewer accidents such as injury dehiscence.
In addition, since the V-Y flap also produces a smaller dead space and presents less risk of postsurgery complications, such as sieroma and hematoma. Considering the biomechanical principles, the modified V-Y flap of which is presented technique is mainly aimed at avoiding the distortion of the flap, placing the adaptation of the epidermal surfaces of the wound seamlessly. Ultimately, the modified V-Y flap of which the technique is described guarantees an undistorted flap that can slide to the maximum possible position by aligning the margins of the skin wound directly adjacent to each other with consequently favorable forces of vector distribution of the tension along the margins of the wound. The AA used a 3/0 or 4/0 Monosyn monofilament absorbable suture with detached stitches with nodes spaced less than 1.5 cm apart.
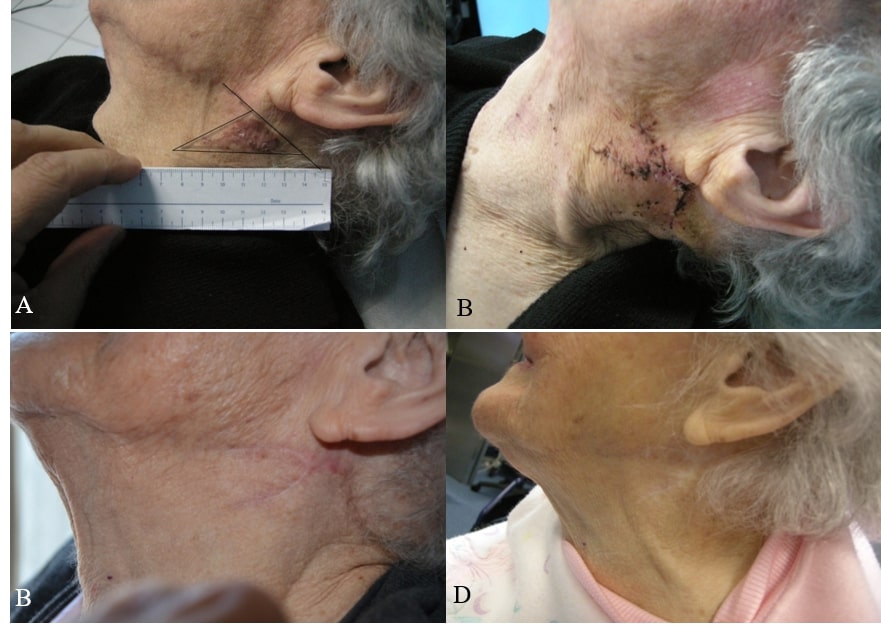
Figure 2: Preoperative conditions and postoperative and follow-up results.
(A) Preoperative drawing in a patient presenting with a neoplastic lesion (Basal cell carcinoma) of flattened triangular shape. (B) Postoperative situation at 7 days after surgery at suture removal (suture material used: 3/0-4/0 resorbable monofilament). (C) Post-operative result at 3 months after surgery; Note that the scar is T-shaped. (D) Scar appearance at 4 months after surgery.In addition, the use of sterile strips and/or tissue glue is recommended for optimal results.
The preoperative representation and post-operative results are shown in Figure 2 A-D.
Antibiotics (levofloxacin 500 mg cp) were prescribed once daily for 5 days.
The sutures were removed after 7 days.
Discussion
Ideally, the stitches provide provisional support to the injury until the traction of the newly formed scar tissue strength resists the intrinsic tension of the skin, to prevent secondary enlargement of the scar. Both the operating surgeon and the patient contribute significantly to the results even if “identical” suture techniques and identical flap patterns are used.
Moreover, even with a comprehensive literature review, there is not enough evidence to determine whether a particular technique for primary wound closure is better than others. And yet, especially with indications in cosmetic plastic surgery, expectations for minimal, hidden or “invisible” scars remain high.
In this regard, the common principles of the patch of skin include: (i) the choice of the smallest suture that can adequately hold the wound edges during healing and can achieve a near absence of closing tension; (ii) that the tensile strength must correspond to the tensile strength of the respective tissue; (iii) that, as the injury heals, the relative loss of suture forces of the limb over time should be slower than that of the limb itself the tissue tensile strength gain for scar formation and (iv) minimize tissue trauma caused by surgical manipulation.
These principles are well known [12] and are therefore not the subject of further discussion here.
The technique of the modified V-Y flap with a horizontal branch (V-T flap), presented is intended to optimize and improve existing techniques to obtain the best post-operative scar with emphasis on the aesthetic result. This can be particularly advantageous in wounds of the face and neck with high resistance to forces.
Furthermore, the technique presented is not destined to replace the classic V-Y flap but is intended to be an alternative for those elongated lesions that, located especially on the face and neck, make it difficult to use the conventional flap [13,14].
Ultimately, we recommend our modified technique when a seamless, low-voltage wound adaptation is desired to achieve the best aesthetic results or in situations of considerable distracting tensile forces or variable wound thickness opposite the margins, especially in those neoplasms that present with a non-discoidal shape. Our VY flap did not require postoperative refinement such as scar revision, debulking or dermabrasion.
Conclusion
Although there are various methods for reconstructing cutaneous imperfections created by resection of a skin cancer, we believe that the modified horizontal VY advancing stratum produces a good treatment result in conditions with small to medium defects particularly in those asymmetric areas subject to tension. In addition, the use of the unilateral VY advancement flap can be extended not only for circular or elongated facial defects, as in our case, but also on the trunk and ends. The advantages of this local flap compared to other local flaps are fewer scars and higher aesthetic results, which are due to the lower scarification of adjacent normal tissues and because it is a simple surgical procedure.
The modified VY flap is an abundant flap that can be used to repair a wide variety of facial defects with elegance and minimal procedural morbidity. The flap repairs wounds with a skin of excellent color and tissue correspondence. The branch VY advancement flap (V-T flap) should be considered an ideal reconstructive choice for soft tissue defects of the face and cheek of a non-round shape. The authors argue that the flap cannot be considered a valid choice for the distal nose reconstruction defects, the flap can be problematic on the bottom of the nose if the mobility of the nasal skin is limited or evaluated erroneously. In this case, prominent nasal distortion may occur after inadequate flap advancement as secondary tissue movement is required to close the primary surgical defect.
Compliance with ethical standards
Declaration of interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding: This research did not receive any specific grant from funding agencies in public, commercial, and not-for-profit sectors.
Availability of data: The datasets collected and\or analyzed during the current study are available from the corresponding author on request. The corresponding author had full access to all the data in the study and takes the responsibility for the integrity of the data and the accuracy of the data analysis.
Ethics approval and consent to participate: All the performed procedures were in accordance with the ethical standards of our institutional research committee, and with the 1964 Helsinki declaration and its later amendments. A written informed consent has been obtained from our patient.
References
- Bichakjian C, Armstrong A, Baum C, Bordeaux JS, Brown M, et al. Guidelines of care for the management of basal cell carcinoma. J Am Acad Dermatol. 2018; 78: 540-559.
- Bader RS. Basal Cell Carcinoma Clinical Presentation. Medscape. 2020.
- Accardo G, Aveta A, Ambrosino E, Aceto B, Di Martino A, et al. A surgical algorithm for partial or total eyebrow flap reconstruction. J Surg Oncol. 2015; 112: 603-9.
- Li JH, Xing X, Liu HY, Li P, Xu J. Subcutaneous Island pedicle flap: variations and versatility for facial reconstruction. Ann Plast Surg. 2006; 57: 255-259.
- Kwon KH, Lee DG, Koo SH, Jo MS, Shin H, et al. Usefulness of v-y advancement flap for defects after skin tumor excision. Arch Plast Surg. 2012; 39: 619-625.
- Hairston BR, Nguyen TH. Innovations in the island pedicle flap for cutaneous facial reconstruction. Dermatol Surg. 2003; 29: 378-385.
- Tateo A, Tateo S, Bernasconi C, Zara C. Use of V-Y flap for vulvar reconstruction. Gynecol Oncol. 1996; 62: 203-207.
- Tavares E, Castellano DP, Rosa J. Retalho de avanço V-Y de pedículo proximal para encerramento de defeito cirúrgico do dorso da mão. Rev Soc Port Dermatol Venereol. 2012; 70: 345-347.
- Christen T, Koch N, Philandrianos C, Ramirez R, Raffoul W, Beldi M, et al. The V-Y latissimus dorsi musculocutaneous flap in the reconstruction of large posterior chest wall defects. Aesthetic Plast Surg. 2012; 36: 618-622.
- Nursal TZ, Ezer A, Calişkan K, Törer N, Belli S, Moray G. Prospective randomized controlled trial comparing V-Y advancement flap with primary suture methods in pilonidal disease. Am J Surg. 2010; 199: 170-177.
- Gardner ES, Goldberg LH. Eyebrow reconstruction with the subcutaneous island pedicle flap. Dermatol Surg. 2002; 28: 921- 925.
- Tavares E, Defeito Medial da Sobrancelha: Reconstrução com Retalho Pediculado de Avanço V-Y, Gazeta Médica. 2019; 6:192- 197.
- Putri SA, Fitra YJ, Kurniadi. V-Y Nasolabial Flap for Reconstruction After Basal Cell Carcinoma Excision, CDK-305. 2022; 49: 6.
- Kwon KH, Lee DG, Koo SH, Jo MS, Shin H, Seul JH. Usefulness of V-Y Advancement Flap for Defects after Skin Tumor Excision. Archives of Plastic Surgery. 2012, Georg Thieme Verlag KG.